

Genital warts affect the moist tissues of the genital area. They can look like small, flesh-colored and be flat or bumpy or have a cauliflower-like appearance. Some genital warts are so small they cannot be seen. They can cause pain, discomfort or itching. Genital warts, also known as venereal warts, or condylomata acuminata, are caused by the human papilloma virus (HPV). More than 100 types of HPV are known to exist. Low risk types (HPV 1, 2, and 3) cause warts on the hands, feet, and other parts of the body. The low risk strains - Types (6 and 11) can cause warts on the genitals or anus (genital warts), and other high risk strains - Types (HPV 16 and 18) can cause cancer of the cervix, external genitalia, vulva, and anus.
Genital warts are sexually transmitted disease (STD) and all partners should be checked thoroughly. They can also be seen in infants who have been delivered vaginally to mothers with HPV in their genital tracts; therefore, alternate methods of delivery should be considered.
Only a small percentage of people infected with HPV will develop genital warts. Many people are carriers of HPV who may never develop warts, but may still be able to pass HPV to their sexual partners. The incubation period from contracting HPV until the development of warts may be several months although some people may not develop warts for years after contact with HPV. People who have lower immunity due to cancer, AIDS, organ transplantation, immune suppressive medications, or certain other medications are more susceptible.
To diagnose this condition, your doctor will do the following:
Although HPV isn't curable in all cases, genital warts are treatable. You can also go extended periods of time without an outbreak, but it may not be possible to get rid of the warts forever. That's because genital warts are only a symptom of HPV, which may become a chronic, lifelong infection for some.
If you've developed genital warts, your doctor has a few options for treatment. The fastest way to remove them is through surgery or to freeze them off with liquid nitrogen. Some doctors might use an electric current or laser treatment to burn off the warts.
Genital warts can go away with treatment from your healthcare provider or with prescription medicine. If left untreated, genital warts may go away, stay the same, or grow in size or number. Cervical precancer treatment is available.
Your doctor may apply a mild acidic solution, called an acetowhite test, to your skin to help make genital warts more visible. It may cause a slight burning sensation.
If you have a vulva, your doctor may also need to perform a pelvic examination, because genital warts can occur deep inside your body.
While visible genital warts often go away with time, HPV itself can linger in your skin cells. This means you may have several outbreaks over the course of your life.
So managing symptoms is important because you want to avoid transmitting the virus to others. That said, genital warts can be passed on to others even when there are no visible warts or other symptoms.
You may wish to treat genital warts to relieve painful symptoms or to minimize their appearance. However, you can’t treat genital warts with over-the-counter (OTC) wart removers or treatments.
Your doctor may prescribe topical wart treatments that might include:
If visible warts don’t go away with time, you may need minor surgery to remove them. Your doctor can also remove warts through these procedures:
To help prevent genital warts, HPV vaccines, condoms, and other barrier methods are available:
If you think you have genital warts, talk with your doctor. They can determine if you have warts and what your best treatment options are.
In addition, it’s important to talk with your sexual partner. This may sound difficult, but being open about your condition can help you protect your partner from also getting an HPV infection and genital warts.
Genital warts are a complication of a low risk HPV infection that’s common and treatable. They can disappear over time, but treatment is essential in preventing their return and possible complications.
Does your torn or expanding earring hole(s) cause you to worry about loosing an earring? If you are feeling limited because the hole is too big to accommodate some of your favorite earrings then Earlobe repair may be a solution for you. It is an easy in office procedure that restores your earlobe in about 30 minutes.
The dermatology practice of Bruce Robinson, M.D., offers advanced procedures including earlobe repair to not only improve your profile but restore self-confidence. If you would like to learn more about this exciting procedure or any of our other services, contact us today to schedule your initial consultation!
All patients have very distinctive reasons for considering earlobe repair. Accidents can occur at any given time in one’s life that may result in traumatized tissue. An earring could get caught up in a piece of clothing and cause a tear. Heavy or large jewelry can lead to stretched or enlarged earlobes with consistant wear. Whatever your reason may be, earlobe repair surgery can be performed to either remedy the earlobes natural appearance or to correct a tear, stretch, scar, or damage from a previous piercing or accident.
Usually 6 - 8 weeks you can re-pierce your ear(s). We offer ear piercing in our office.
We use the Coren PS ear piercer which painlessly pierces your earlobes and inserts a sterile, hypoallergenic, 24k gold ear stud.
Link to ear piercing instruction sheet
A cyst is a closed sac with a defined membrane and division on the nearby tissue.
Cysts may contain fluid, air or semisolid material. Parasites — such as trichinosis, dog tapeworm and echinococcus. Cysts are typically benign growths that consist of a wall that makes the contents. Often these bumps are cosmetically unacceptable or patients desire removal in the event they may rupture. Although cysts can remain intact for a lifetime, may go away on their own.There is also the risk of rupturing, which can lead to a great deal of inflammation, pain and infection. This necessitates surgical excision.
Sebaceous / Epidermoid Cysts are typically a common, noncancerous type of cyst. Sebaceous cysts arise from sebaceous glands that secrete oily matter that lubricates the hair and skin. These cysts, which may be hereditary, are caused when glands or hair follicles become blocked. Trauma to the skin is another likely cause of a cyst. These cysts appear as small bumps beneath the skin. Although they can occur almost anywhere on the body, they typically appear on the face, neck and trunk. A foul odor may be secreted from the outside skin of the cyst. Sebaceous cysts grow slowly and usually are not painful; thus, treatment is rarely needed. However, options are available if these cysts become painful or have an unacceptable appearance.
There are three common cyst removal techniques specifically for sebaceous cysts — conventional wide excision, minimal excision and punch biopsy excision.
Lastly, these cysts typically appear on the scalp which originate in the skin and hair follicles, may cause lumps under the skin, but often do not require surgical removal.
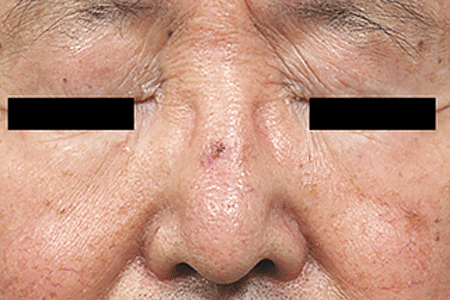
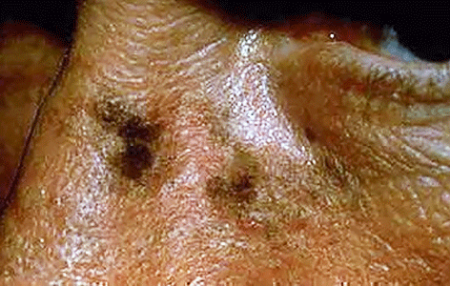
An atypical nevus or dysplastic nevus (mole) is a benign growth that may share some of the features of a melanoma, but is NOT a melanoma or any other form of cancer. The presence of an atypical nevus, however, may increase the risk of developing a melanoma, or be a marker for it. A single atypical nevus may indicate a small risk; this risk increases with the number of atypical nevi present.
An atypical nevus can vary in appearance. Since it has the ABCDE features of a melanoma, it is important ot have a dermatologist examine all moles.
Asymmetry - One half does not match the other half in size, shape, color, or thickness.
Border irregularity - The edges are ragged, scalloped, or poorly defined.
Color - The pigmentation is not uniform. Shades of tan, brown, and black are present. Dashes of red, white, and blue add to the mottled appearance.
Diameter - While melanomas are usually greater than 6mm in diameter (the size of a pencil eraser) when diagnosed, they can be smaller. If you notice a mole different from others, or one which changes, itches, or bleeds (even if it is small), you sould see a dermatologist.
The lifetime risk of a person in the United States developing melanoma is 1 in 75. A patient with one to four atypical nevi without a personal or family history of melanoma is at a slightly higher risk than the general population. The risk of developing melanoma is higher if a patient with atypical nevi has a personal or family history of melanoma. A patient who has multiple atypical and normal nevi (moles) may have Familial Atypical Nevus Syndrome, and is at an increased risk for developing a melanoma, especially if a relative had melanoma.
Where and when do atypical nevi occur?
Atypical nevi begin to appear at puberty and can occur anywhere on the body, but are more common in sun-exposed areas, the back, and the legs.
Since an atypical nevus is not the same as a melanoma, it does not need to be treated aggressively but should be observed for changes, biopsied, or conservatively excised.
Familial Atypical Nevus Syndrome
The National Institute of Health Consensus Conference defines the Familial Atypical Nevus Syndrome as those persons meeting the following criteria:
It is important for people with Familial Atypical Nevus Syndrome to have a full body screening from a dermatologist every three to twelve months beginning with the onset of puberty. The dermatologist might also recommend regular ophthalmologic examinations, baseline skin photography, or regular screenings of relatives to permit early detection and treatment of melanoma since detection in the early stages has a much higher cure rate.
People with Familial Atypical Nevus Syndrome should also examine their own skin every month. When performing self-examinations, be aware of any lesions that appear to change in size, color, and/or shape. If a change has occurred, bring this to the attention of a dermatologist immediately. Information on the early signs of melanoma is available from the dermatologist or the American Academy of Dermatology.
Prevention of Melanoma
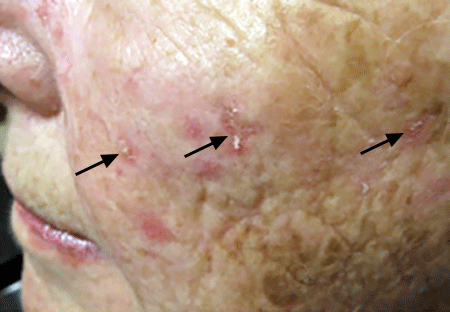
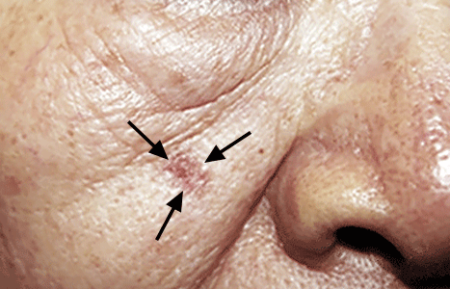
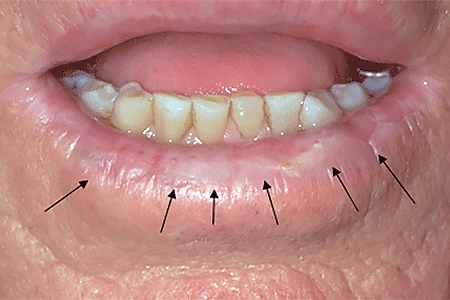
An actinic keratosis, is a rough, scaly patch on the skin that develops from years of sun exposure. It's often found on the face, lips, ears, forearms, scalp, neck or back of the hands. These represent pre-cancerous growths that can become skin cancer if left untreated.
If you find a spot or growth on your skin that you think could be an actinic keratosis (AK), it’s time for a thorough skin exam. Should you have an AK, an accurate diagnosis and treatment can:
Most people who have AKs (or think they may have an AK) see a dermatologist. This is actually one of the most common conditions that dermatologists diagnose and treat.
When you see a board-certified dermatologist about AKs, your dermatologist will:
If you have one or more AKs on your skin, a board-certified dermatologist can often diagnose you by looking carefully at your skin. While examining your skin, your dermatologist will also look for signs of skin cancer. People who have skin that’s been badly damaged by ultraviolet (UV) light develop AKs and have a higher risk of getting skin cancer.
If you have one or more AKs, your dermatologist will talk with you about whether to treat these precancerous skin growths. Usually, treatment is recommended.
For a few people, a dermatologist may recommend frequent skin exams rather than treatment. Skin exams are recommended for patients who are frail and may find it hard to tolerate treatment. To be effective, treatment must destroy the AKs. When this happens, your skin will feel raw. It may be red and swollen for a brief time.
The treatment that is right for you depends on several considerations, including:
If you have one or a few AKs, a procedure that your dermatologist can perform during an appointment may be the preferred treatment.
You can often complete treatment in 1 or 2 office visits. The procedures that dermatologists use to treat AKs include:
Some people develop a few AKs, which can often be cleared with treatment.
If you have many AKs, it’s a good idea to be under a dermatologist’s care. Your skin has been severely damaged by UV light, so it’s likely you’ll continue get new AKs. You may also develop skin cancer. Your dermatologist can watch for signs of new AKs and skin cancer. When found early and treated, skin cancer is highly treatable.
Your dermatologist will tell you how often to return for check-ups. Some people need a check-up once or twice a year. If you have a weakened immune system or a rare condition that greatly increases your risk of developing AKs and skin cancer, you may need to see your dermatologist every 8 to 12 weeks.
Keep every appointment. If skin cancer develops, the sooner it is found and treated, the better your outcome.
Self-care also plays a key role in your outcome. The right self-care can help to prevent new AKs and skin cancer.


Acne is a skin condition which has plugged pores (blackheads and whiteheads), inflamed pimples (pustules), and deeper lumps (nodules). Acne occurs on the face, as well as the neck, chest, back, shoulders, and upper arms. Although most teenagers get some form of acne, adults in their 20's, 30's, 40's, or even older, can develop acne. Often, acne clears up after several years, even without treatment. Acne can be disfiguring and upsetting to the patient. Untreated acne can leave permanent scars; these may be treated by your dermatologist in the future. To avoid acne scarring, treating acne is important.
Acne is not caused by dirt. Testosterone, a hormone which is present in both males and females, increases during adolescence (puberty). It stimulates the sebaceous glands of the skin to enlarge, produce oil, and plug the pores. Whiteheads (closed comedones), blackheads (open comedones), and pimples (pustules) are present in teenage acne.
Early acne occurs before the first period and is called prepubertal acne. When acne is severe and forms deep "pus-filled" lumps, it is called cystic acne. This may be more common in males. Adult acne develops later in life and may be related to hormones, childbirth, menopause, or stopping the pill. Adult women may be treated at the period and at ovulation when acne is especially severe, or throughout the entire cycle. Adult acne is not rosacea, a disease in which blackheads and whiteheads do not occur.
Acne has nothing to do with not washing your face. However, it is best to wash your face with a mild cleanser and warm water daily. Washing too often or too vigorously may actually make your acne worse.
Acne is not caused by foods. However, if certain foods seem to make your acne worse, try to avoid them.
Wear as little cosmetics as possible. Oil-free, water-based moisturizers and make-up should be used. Choose products that are "non-comedogenic" (should not cause whiteheads or blackheads) or "non-acnegenic" (should not cause acne). Remove your cosmetics every night with mild soap or gentle cleanser and water.
A flesh-tinted acne lotion containing acne medications can safely hide blemishes. Loose powder in combination with an oil-free foundation is also good for cover-up.
Shield your face when applying sprays and gels on your hair.
Control of acne is an ongoing process. All acne treatments work by preventing new acne breakouts. Existing blemishes must heal on their own, and therefore, improvement takes time. If your acne has not improved within two to three months, your treatment may need to be changed. The treatment your dermatologist recommends will vary according to the type of acne.
Occasionally, an acne-like rash can be due to another cause such as make-up or lotions, or from oral medication. It is important to help your dermatologist by providing an updated history of what you are using on your skin or taking internally.
Many non-prescription acne lotions and creams help mild cases of acne. However, many will also make your skin dry. Follow instructions carefully.
Re-think your skin health. Hydrafacial MD, - * Acne Facial, is highly effective for anyone suffering from oily and/or acne-prone skin. It visibly reduces redness, enlarged pores, hyperpigmentation, utilizing LED blue light killing acne causing bacteria. HydraFacial MD - Hydradermabrasion is the latest, non-invasive, "gentle" skin resurfacing and complexion treatment. The immediate, noticeable, long lasting results are achieved with zero downtime and without any discomfort. You can return to school, work, social life, or exercise right after your procedure. HydraFacial MD uses a uniquely shaped spiral tip and patented vortex fusing technology to gently cleanse, exfoliate, and extract, removing impurities and dead skin cells while hydrating the skin and adding antioxidant protection simultaneously.
Acne scars no longer have to be lived with forever. Often occurring on the face, back and chest these scars can now be treated with a variety of lasers (Fraxel®, V-Beam), subcission or chemical peels. These treatments require no social downtime and can be performed on all skin colors.
A surgical excision is an in-office procedure in which a skin lesion is removed by a dermatologic surgeon. This technique involves the use of local numbing medicine which is injected into and around the target area and followed by sharp dissection of the lesion from surrounding normal tissue. The most common scenarios for utilization of this technique include: treatment of skin cancers, atypical or suspicious moles (nevi), and cysts.
Cysts may remain asymptomatic, but if they continue to grow or become painful surgical excision is the treatment of choice. The cyst consists of a wall that makes the contents. To insure that the cyst does not return, it is best to completely excise it, including the wall, to prevent its recurrence.
Moles often become more raised over time. Occasionally they become irritated or are cut when shaving. A shave excision removes the raised portion of the mole. As a general rule, a complete excision is only performed if a mole is changing or when a complete excision will yield a better cosmetic result. Either of these treatments is performed under local anesthesia in our office. The shave excision takes less than a minute and a complete excision under a half hour. The functional and cosmetic results are excellent.
This option is typically for scars that are deeply pitted, raised, or for older surgical scars that did not heal properly. The scar tissue is removed, followed by careful stitching of the skin to leave a much smaller, thinner scar line or to change the scars shape and/or direction so it is less obvious.
Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
What is intralesional steroid injection used for?
Intralesional Steroid Injections, or Intralesional Kenalog is a common treatment used in dermatology & are a standard treatment for many skin diseases including: acne lesions, cysts, alopecia (bald spots) hair loss, eczema, abundant scar tissue (keloids, hypertrophic scars), psoriasis, lichen simplex chronicus, skin lupus, granuloma annulare, and more. Intralesional injections are extremely helpful, as they are able to bypass the outer defensive layers of the skin to reach an area that will make the greatest impact on your condition. It is common for a patient to need multiple injections, as different cases vary in severity. The goal of these injections is ideal for quick healing to reduce the inflammation within the skin, and relive pain and discomfort as well as improving the appearance. This treatment is usually reserved for tender, swollen acne nodules, or cysts that aren't responding to typical acne therapies. Prompt treatment with intralesional injections can often prevent scarring.
Torn, split or long and droopy earlobe rejuvenation is an easy in-office procedure that takes approximately 30 minutes from start to finish. Under local anesthesia an enlarged earring hole is closed or a torn earlobe is restored. The sutures are removed in just one week. Dr. Robinson can re-pierce your ears 6 weeks later (https://brucerobinsonmd.com/earlobe-piercing/). So go ahead and get those earrings you always wanted but couldn't wear.
Yes! While a torn earlobe can be painful and distressing, an expert dermatologist like Dr. Bruce Robinson can effectively repair it with just a few precise sutures. Using advanced cosmetic surgical techniques, Dr. Robinson ensures a clean repair that typically heals into a small, barely noticeable scar. About three months after the procedure, patients can return for professional re-piercing. Dr. Robinson carefully places the new piercing at a safe distance from the repaired area to prevent any further damage.
The first step in repairing a torn earlobe is a consultation with experienced, board-certified dermatologist Dr. Bruce Robinson. He will thoroughly evaluate the damage and determine if you’re a good candidate for earlobe repair. Listening closely to your cosmetic goals, Dr. Robinson will develop a personalized treatment plan tailored to your needs.
The procedure is performed safely in-office without sedation or general anesthesia. Dr. Robinson will numb the earlobe with local anesthesia to ensure your comfort throughout the treatment. He will then carefully remove any scar tissue around the tear and expertly suture the wound closed. The exact technique used depends on the severity of the tear, whether it’s a minor split or a complete rupture. For patients with sagging earlobes, Dr. Robinson may also use hyaluronic acid fillers like Juvederm or Restylane to restore volume and lift.
After the procedure, Dr. Robinson will provide detailed post-care instructions. Most patients only need over-the-counter pain relief, such as Tylenol, if any discomfort arises. Sutures are typically removed two weeks post-treatment, and approximately three months later, patients can return for safe and precise earlobe re-piercing. Dr. Robinson ensures the new piercings are symmetrical and positioned to avoid further damage to the repaired area.
Sagging or stretched earlobes can result from various factors. Tears or injuries, frequent wearing of heavy earrings, and even sleeping with earrings can stretch the delicate skin, causing earlobes to sag over time. Additionally, natural aging reduces collagen and elastin production, proteins essential for skin firmness and elasticity leading to loss of volume and drooping earlobes.
Dr. Robinson offers a non-surgical solution to restore lost volume and firmness using dermal fillers like Restylane and Juvederm. These fillers contain hyaluronic acid, a naturally occurring substance that enhances skin hydration and volume. Injecting these fillers into the earlobes improves elasticity and helps support earrings comfortably.
The earlobe filler treatment is quick, simple, and minimally uncomfortable. A topical numbing cream is applied about an hour before your appointment to reduce any discomfort. Once in the office, the area is cleaned and sterilized before Dr. Robinson expertly injects the chosen filler to rejuvenate your earlobes. After the procedure, ice is applied to minimize swelling or bruising.
Mild redness, swelling, or bruising may occur but typically resolve within a few days. To reduce bruising, patients prone to it can take oral Arnica supplements before and after treatment. It’s also recommended to avoid blood thinners such as NSAIDs, fish oil, and vitamin E for one week before and after the procedure.
Dermal fillers provide a safe and effective, non-invasive way to restore volume and durability to sagging earlobes. Results usually last about six months, depending on the filler used.
Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
The Coren PS earpiercer painlessly pierces your earlobes and inserts a sterile, hypoallergenic, 24k gold ear stud.

