We are pleased to introduce ProNox™ in our practice, a patient controlled, inhaled analgesia for in-office use. We want our patients to achieve their cosmetic goals worry-free. Patients say that it has made all the difference in moving forward with many cosmetic procedures.
The use of nitrous oxide in Medical, Cosmetic & Laser Dermatologic procedures is becoming more common. Our goal is to provide each patient with a pain-free experience and to work with their varied anxiety levels. While we have excellent topical numbing options for pain control, nitrous oxide can help calm the patient who is nervous or anxious and also help with pain relief.
So many of us struggle from natural hair thinning and hair loss. In fact, according to the International Society of Hair Restoration Surgery, approximately 56 million adults in the United States are affected by hair loss. Different conditions can lead to different symptoms of hair loss, ranging from male pattern baldness, which is characterized by hair loss at the temples followed by thinning along the crown, to thinning or loss that can occur in patches throughout the scalp. Hair loss or hair thinning can occur in both men and women and can be a source of self-consciousness or embarrassment and, up until recently, few non-surgical treatments offered total hair restoration.
Recently, Platelet-Rich Plasma (PRP) has become a popular regenerative treatment in the world of dermatology. PRP treatment for hair restoration, is not a permanent solution for hair regrowth, but it can help to slow down the progression of hair loss and promote new growth in areas where there was previously none. It can offer significant improvements in hair thickness, density and reduces hair shedding. The treatment takes platelet-rich plasma from the patient’s own blood and once isolated, the PRP solution is injected into the area affected by hair loss or hair thinning. The PRP triggers the natural hair growth process and strengthens the hair follicles to promote regrowth and prevent hair loss. The procedure is simple and requires minimal downtime or discomfort, making it an excellent option for patients who are wary of surgical options, such as hair transplants.
Board-certified dermatologist Dr. Bruce Robinson is an expert in PRP treatment and was one of the first dermatologists to incorporate PRP into his private NYC practice. PRP has been a boost to patients with hair loss, delivering improved hair growth and hair thickness with his PRP hair restoration patients. Experienced dermatologist, Dr. Bruce Robinson, has been treating patients in his Upper East Side, New York City office for more than 30 years and is an expert in a range of cosmetic and dermatological procedures. If you’re frustrated by thinning hair or hair loss, Dr. Robinson is here to help.
Therapy for hair loss is a three-step medical treatment in which a person's blood is drawn, processed, and then injected into the scalp. Platelet-rich plasma is a concentration of platelets that is 3x the normal blood value, and contains many growth factors that stimulate hair follicles and can safely be performed up to every month, based on how much hair growth is required. PRP is a great solution for hair loss in both men and women, especially when hair transplant surgery is not an option. PRP injections can stimulate new hair growth in men who suffer from androgenetic alopecia (known as male pattern baldness) and women who suffer from female pattern baldness.
The Platelets in the PRP contain proteins that are needed in order to promote the rate of tissue healing and regeneration within inactive hair follicles. Inside these platelets are a variety of intracellular structures such as glycogen (a form of glucose), lysosomes (which break down the proteins), and alpha granules (which contain clotting and growth factors that get released during the cell repair process). Platelet-rich plasma-derived growth factors can also play a part in stem cell differentiation within the wound healing process of the musculoskeletal system.
In multiple studies through the Journal of Cosmetic Dermatology and Aesthetic Plastic Surgery, patients suffering from hair loss were found to benefit from PRP injections. The PRP hair restoration treatment led to a significant local increase in hair number, extended growth phase, and improved hair thickness. Though the treatment is not yet FDA-approved, there is scientific proof that the treatment is beneficial for hair strength and new hair growth at and around a PRP injection site.
The science behind PRP uses proven benefits of PRP to naturally promote new cellular growth. PRP is directly involved in regenerative healing within the body. PRP growth factors can thus influence hair growth and can in fact restore hair follicles, in turn improving the look and feel of a patient’s hair.
PRP hair rejuvenation treatment involves the injection of platelets into the area of the body in which hair loss is occurring, for example the crown of the head. Platelets are taken from the patients own body via a blood draw that occurs at the start of the appointment. After the blood has been drawn, it is placed in a centrifuge, which is a machine that separates the platelet-rich plasma from the red blood cells. When isolated, the platelet-rich plasma is then injected into the treatment area. The platelets release growth factors, which stimulates the dermal papilla cells that are crucial in the hair growth process. For that reason, a series of PRP injections help to trigger hair regrowth to restore lost hair.
Though of course the number of PRP treatments varies depending on the hair condition and aesthetic goals of the individual patient, a typical patient will do three sessions of PRP therapy. Further treatments will be evaluated at the end of the fourth month (after the third PRP treatment).The sessions are typically spaced 4-6 weeks apart, and Dr. Robinson personally performs all consultations and injections. PRP treatments can also be used in tandem with hair transplantation to help accelerate hair growth. At your initial consultation with Dr. Robinson, you will be able to discuss all hair treatment options, including PRP injections. Dr. Robinson will use his expertise to provide the best medical advice, diagnosis, and treatment available for hair loss.
Unfortunately, as PRP hair restoration is considered a cosmetic procedure, PRP for hair loss is not covered by health insurance. For more information, it’s best to contact your insurance company directly to ascertain coverage.
Many patients come into their initial consultation with Dr. Robinson wondering, how fast does PRP work for hair loss? Of course, any results will vary depending on the nature of hair loss and desired results of each patient. However, the majority of patients see initial improved hair thickness and hair growth several weeks after treatment. Optimal results from PRP injections are apparent, on average, about 5-6 months after treatment.
A good candidate for PRP hair restoration is a patient who is showing signs of thinning hair or hair loss. Typically, candidates who have experienced hair loss more recently, or who are dealing with early hair loss, respond best to PRP hair treatment. Those with hair follicles that have been dormant for longer on the scalp are less likely to be improved by PRP therapy. It’s good to note that if you are diagnosed with a underlying disorder such as lupus or thyroid disease, you are unlikely to benefit form PRP injections, as these conditions will continue to worsen hair loss over time. Additionally, patients should not take blood thinners during PRP hair restoration treatment, as the procedure will be significantly less effective.
Call today to schedule an appointment with Dr. Robinson.
Telangectasias (commonly known as spider veins) are dilated or broken blood vessels located near the surface of the skin. They often occur on the face and particularly on the sides of the nose. They often look like small red or pink lines, which temporarily whiten when pressed.
Some Symptoms Of Spider Veins Include:
Common Causes of Spider Veins
Spider veins are generally caused by weak or damaged valves. The following causes can contribute to weaker blood flow in certain areas of your body.
Treatment(s):
Thankfully, laser therapy is safe and efficacious treatment. It is an easy in-office treatment that can be performed during ones lunch break. In 10 minutes those red lines are gone and you can go right back to work. No wound care or dressings needed.
Sclerotherapy is also a treatment option. A special solution is injected directly into the affected veins, forcing the veins to close and the blood to redirect into healthier veins. The old vein turns into scar tissue that your body will eventually absorb, causing it to fade.
Subcission is a treatment used to correct a type of scar called a valley scar. A valley scar simply means there is a defect in the volume of the skin at the site of the scar. The goal of subcission is to improve this decreased volume. This then allows a depressed scar to regain its smooth appearance. This treatment may be combined with other scar treatments to yield the best cosmetic results.
Squamous cell carcinoma is the second most common cancer of the skin. More than 250,000 new squamous cell carcinomas are diagnosed every year in the United States. Middle-aged and elderly people, especially those with fair complexions and frequent sun exposure, are most likely to be affected.
The cancer develops in the outer layer of the skin (the epithelium). Some squamous cell carcinomas arise from small sandpaper-like lesions called solar (sun) or actinic keratosis. It is possible for squamous cell carcinoma to spread to other areas of the body; therefore, early treatment is important.
Squamous cell carcinomas usually appear as crusted or scaly patches on the skin with a red, inflamed base, a growing tumor, or a non-healing ulcer. They are generally found in sun-exposed areas like the face, neck, arms, scalp, backs of the hands, and ears. The cancer also can occur on the lips, inside the mouth, on the genitalia, or anywhere on the body. Any lesion, especially those that do not heal, grow, bleed, or change in appearance, should be evaluated by a dermatologist.
Ultraviolet light exposure (from the sun or indoor tanning devices) greatly increases the chance of developing skin cancer. Although anyone can get squamous cell carcinoma, people with light skin who sunburn easily are at the highest risk. The chance of developing skin cancer increases with age and a history of severe sunburns as a child. Many less common skin conditions, organ transplantation, chronic skin ulcers, prior x-ray treatment (e.g., for acne in the 1950s), arsenic ingestion, smoking, and toxic exposure to tars and oils can predispose individuals to the development of squamous cell carcinoma.
These skin cancers are usually locally destructive. If left untreated, squamous cell carcinoma can destroy much of the tissue surrounding the tumor and may result in the loss of a nose or ear, for example. Aggressive types of squamous cell carcinomas, especially those on the lips and ears, or untreated cancers, can spread to the lymph nodes and other organs resulting in approximately 2,500 deaths each year in the United States.
A skin biopsy for microscopic examination may be done to confirm the diagnosis. A variety of different treatment options can be used depending on the location of the tumor, size, microscopic characteristics, health of the patient, and other factors. Most therapies are relatively minor office-based procedures that require only local anesthesia. Surgical excision to remove the entire cancer is the most commonly used treatment. "Mohs" micrographic controlled surgery, a method which requires specialized training by dermatologic surgeons, can be used to remove the tumor while sparing as much normal skin as possible. Other dermatologic surgical procedures include laser surgery, cryosurgery (liquid nitrogen - the frozen method), radiation therapy, and electrodesiccation and curettage which involves alternately scraping and cauterizing (burning) the tumor with low levels of electricity.
Skin Cancer is the cancer you can see! Yet skin cancer often goes undetected. With over 5 million cases of skin cancer diagnosed in the U.S. each year, skin cancer is America's most common cancer. More people are diagnosed with skin cancer each year in the U.S. than all other cancers combined.
Types of skin cancers include: Basal Cell Carcinoma, Squamous Cell Carcinoma, Melanoma and Merkel Cell Carcinoma, they are mainly caused by UV exposure to ultraviolet (UV) radiation from the sun. However, skin cancer can form anywhere on the body even if it is not exposed to the sun. All ethnicities and skin tones are at risk.
Dr. Bruce P. Robinson has pioneered a transformative new treatment option for the most common forms of skin cancer: Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC). His new and significant research in the treatment of Basal & Squamous cell carcinoma’s can be seen in the Archives of Dermatological Research, Utilizing fractional lasers and tirbanibulin ointment to treat squamous and basal cell carcinomas with a 99% cure rate to date and no recurrence
Basal Cell Carcinoma is the most common skin cancer and the number of reported cases in the U.S. is steadily increasing. It is also one of the easiest to spot and treat. Squamous Cell Carcinoma is the second most common skin cancer and Melanoma the third. Despite Melanoma being the third most common form of skin cancer, it accounts for 75% of all skin cancer deaths.
Squamous Cell Carcinoma is the second most common. An estimated 1.8 million cases are diagnosed each year in the U.S. which translates to about 205 cases every hour. SCC incidence has increased up to 200% in the past three decades.
Melanoma is the third most common and deadly cancers. Early detection is critical! In the past decade (2012-2022) the number of new invasive melanoma cases diagnosed annually increased by 31%. An estimated 197,700 cases of melanoma will be diagnosed in the U.S. in 2022 and 7,650 people will die of melanoma in 2022. (5,080 men & 2,570 women).
Merkel Cell Carcinoma is about three - five times more likely to be deadly than melanoma. Approximately 3,000 new cases of Merkel Cell Carcinoma are diagnosed annually in the U.S.
The good news is that skin cancer can be prevented, and it can almost always be cured when it’s found and treated early.
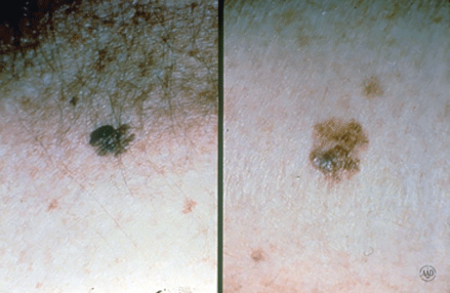
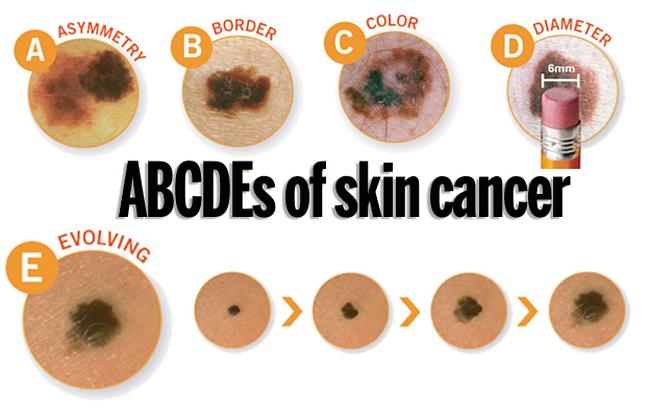
A change in your skin is the most common sign of skin cancer. This could be a new growth, a spot that doesn’t look like others on your body, a sore that doesn’t heal, or a change in a mole. The “ABCDE rule” can be used as a guide. The “ABCDE rule” can be used as a guide (see below).
Skin cancer isn't going to check itself out. Therefore, an annual skin check by a board-certified dermatologist and a monthly skin check by you is vital to good skin care. See something NEW, keep an eye out for any New moles or blemishes that have popped up, CHANGING, a leopard's spots don't change and neither should yours, always check if your spots are Changing in color, size, shape, or texture, or UNUSUAL, one of these things is not like the others ... look for spots that are unusual in outline or continuously itch, hurt, crust or bleed for more than 3 weeks. It could be skin cancer.
When these skin cancers are detected early, treatment often results in a cure. Be sure to schedule an yearly skin exam with your dermatologist and more often if you have a family history of skin cancer.
Take these simple steps today to protect your skin:
Dr. Bruce Robinson is advancing skin cancer treatment with innovative non-invasive techniques that provide superior outcomes compared to traditional methods like surgical excision and Mohs surgery. His approach uses fractional laser technology, which eliminates the need for downtime, scarring, or bleeding, while offering functional and cosmetic results that are more favorable than conventional treatments. This method enhances both patient care and quality of life by reducing the invasiveness of treatment and improving recovery. See Publication Here ...
Skin cancer is the most prevalent cancer in the United States. More than 3 million Americans are diagnosed with non-melanoma skin cancer(s), such as basal cell & squamous cell carcinoma each year. These two types of cancers are collectively known as keratinocyte carcinoma or (KC).
In individuals with a history of a prior KC, the risk of developing subsequent KC remains a significant concern.
Non-ablative fractional laser therapy has already demonstrated remarkable success with minimal downtime & discomfort as a gentle yet effective treatment of actinic keratosis (AK), the most common type of pre-cancerous skin conditions. Other benefits to using non-ablative fractional laser therapy is it's ability @ ameliorating photo damage, utilizing precise photothermolysis to stimulate collagen and elastin production, promote dermal wound healing & decreasing and improving hyperpigmentation, telangiectasias, skin tone, skin laxity, and tactile roughness. Now we can add treatment of certain skin cancers to the list.
Seborrheic Keratoses are often confused with warts or moles, but they are quite different. Seborrheic Keratoses are non-cancerous growths of the outer layer of skin. There may be just one growth or many which occur in clusters. They are usually brown, but can vary in color from light tan to black and range in size from a fraction of an inch in diameter to larger than a half-dollar. A main feature of Seborrheic Keratoses is their "waxy, pasted-on" appearance. They sometimes look like a dab of warm brown candle wax that has dropped onto the skin or like barnacles attached to the skin.
The exact cause of seborrheic keratoses is unknown; however, they seem to run in families. They are not caused by sunlight and can be found on both sun-exposed and non sun-exposed areas. Seborrheic Keratoses are more common and numerous with advancing age. Although Seborrheic Keratoses may first appear in one spot and seem to spread to another, they are not contagious.
Anyone may develop Seborrheic Keratoses. Some people develop many over time, while others develop only a few. As people age, they may simply develop more. Children rarely develop Seborrheic Keratoses. Seborrheic Keratoses may erupt during pregnancy, following estrogen therapy, or in association with other medical problems.
Seborrheic Keratoses are most often located on the chest or back, although they also can be found on the scalp, face, neck, or almost anywhere on the body. The growths usually begin one at a time as small, rough, itchy bumps which eventually thicken and develop a warty surface.
Seborrheic Keratoses are benign (non-cancerous) and are not serious. Unless they develop suddenly, they do not indicate a serious health problem. They may be unsightly, especially if they appear on the face. Removal may be recommended if they become large, irritated, itch, or bleed easily. A Seborrheic Keratosis may turn black and may be difficult to distinguish from skin cancer. Such a growth must be removed and biopsied (studied under a microscope) to determine if it is cancerous or not.
Creams, ointments, or other medication can neither cure nor prevent Seborrheic Keratoses. Most often Seborrheic Keratoses are removed by cryosurgery, curettage, or electrosurgery. Cryosurgery, liquid nitrogen, a very cold liquid gas, is applied to the growth with a cotton swab or spray gun to "freeze" it. A blister may form under the growth which dries into a scab-like crust. The Keratosis usually falls off within a few weeks. Occasionally, there will be a small dark or light spot that usually fades over time.
Curettage: The keratosis is scraped from the skin. An injection or spray is first used to anesthetize (numb) the area before the growth is removed (curetted). No stitches are necessary, and the minimal bleeding can be controlled by applying pressure or the application of a blood-clotting chemical.
Electrosurgery: The growth is anesthetized (numbed) and an electric current is used to burn the growth which is then scraped off.
Today, there are many treatment options which, when properly chosen for the specific type of scar and/or skin type, can greatly improve and repair your skin to its natural and more healthy state. These treatment options include surgical excision, laser skin resurfacing, laser skin rejuvenation, intense pulsed light skin rejuvenation, microdermabrasion, chemical peels, dermabrasion, cortisone injections, and bleaching or age defying softening topicals.
During your consultation, your skin type and scar will be evaluated and a customized treatment program will be developed. This may include a combination of treatments to optimize your results. In some cases, certain types of scars can only be improved and not completely eliminated. Your treatment expectations and results will be thoroughly discussed during your consultation.
This option is typically for scars that are deeply pitted, raised, or for older surgical scars that did not heal properly. The scar tissue is removed, followed by careful stitching of the skin to leave a much smaller or thinner scar line.
This treatment is excellent for acne scarring as well as sun damaged or aged skin. The laser vaporizes the damaged skin and commences the regeneration of fresh skin during the following weeks. The thermal damage to the deep tissue stimulates new skin growth, promoting a healthy new collagen layer as well.
Microdermabrasion is a non-surgical exfoliating treatment helpful for those unhappy with scars, acne scars, sun-damaged skin, pigmentation spots, stretch marks, fine lines, and rough skin. Treatment can be performed anywhere on the body. This treatment works for scarring especially when used in conjunction with other modalities.
This is a non-invasive approach in which the laser energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars.
Depending on the skin type and scar to be treated, a superficial, medium, or deep chemical peel may be recommended. In addition to removing the top layers of the epidermis, chemical peels are noted for their ability to stimulate collagen synthesis and aid in the production of new skin cells. Depending on the type of peel, multiple treatments may be required.
This is a non-invasive approach in which intense pulsed light energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars and coarse, uneven skin texture.
By the time we reach our adult years, our skin has been exposed to rough childhood environmental damage, acne, chicken pox, scrapes, burns and numerous other phenomena. As part of the skin’s natural healing process, a scar is formed when several layers of the skin have been damaged. Presently there are diverse treatment modalities available to address various forms of skin scarring. These treatments can dramatically reverse, improve, and renew your skin to it’s natural, healthier state. Many patients seek solutions not only to achieve healthy-looking skin, but also to improve their image and self esteem.
Everyone has moles, sometimes 40 or more. Most people think of a mole as a dark brown spot, but moles have a wide range of appearance. At one time, a mole in a certain spot on the cheek of a woman was considered fashionable. These were called "beauty marks." Some were even painted on. However, not all moles are beautiful. They can be raised from the skin and very noticeable, they may contain dark hairs, or they may be dangerous.
Moles can appear anywhere on the skin. They are usually brown in color but can be skin colored and various sizes and shapes. The brown color is caused by melanocytes, special cells that produce the pigment melanin. Moles probably are determined before a person is born. Most appear during the first 20 years of life, although some may not appear until later. Sun exposure increases the number of moles, and they may darken. During the teen years and pregnancy, moles also get darker and larger and new ones may appear. Each mole has its own growth pattern. The typical life cycle of the common mole takes about 50 years. At first, moles are flat and tan like a freckle, or they can be pink, brown or black in color, Over time, they usually enlarge and some develop hairs. As the years pass, moles can change slowly, becoming more raised and lighter in color. Some will not change at all. Some moles will slowly disappear, seeming to fade away. Others will become raised far from the skin. They may develop a small "stalk" and eventually fall off or are rubbed off.
Recent studies have shown that certain types of moles have a higher-than-average risk of becoming cancerous. They may develop into a form of skin cancer known as malignant melanoma. Sunburns may increase the risk of melanoma. People with many more moles than average (greater than 100) are also more at risk for melanoma.
Moles are present at birth in about 1 in 100 people. They are called congenital nevi. These moles may be more likely to develop a melanoma than moles which appear after birth. Moles known as dysplastic nevi or atypical moles are larger than average (usually larger than a pencil eraser) and irregular in shape. They tend to have uneven color with dark brown centers and lighter, sometimes reddish, uneven border or black dots at edge. These moles often run in families. People with dysplastic nevi may have a greater chance of developing malignant melanoma and should be seen regularly by a dermatologist to check for any changes that might indicate skin cancer. Those susceptible should also learn to do regular self-examinations, looking for changes in the color, size or shape of their moles or the appearance of new moles. Sunscreen and protective clothing should be used to shield moles from sun exposure. Recognizing the early warning signs of malignant melanoma is important. Remember the ABCDs of melanoma when examining your moles: Read more here for Dr. Robinson in the News on Moles.
Melanoma is the most common type of cancer for young adults 25 to 29 years old, and the second most common type for adolescents and young adults 15-29 years old. Melanoma is a cancer of the pigment producing cells in the skin, known as melanocytes. Cancer is a condition in which one type of cell grows without limit in a disorganized fashion, disrupting and replacing normal tissues and their functions, much like weeds overgrowing a garden. Normal melanocytes reside in the outer layer of the skin and produce a brown pigment called melanin, which is responsible for skin color. Melanoma occurs when melanocytes become cancerous, and then grow and invade other tissues.
Melanoma begins on the surface of the skin where it is easy to see and treat. If given time to grow, melanoma can grow down into the skin, ultimately reaching the blood and lymphatic vessels, and spread around the body (metastasize), causing life-threatening illness. It is curable when detected early, but can be fatal if allowed to progress and spread. The goal is to detect melanoma early when it is still on the surface of the skin.
It is not certain how all cases of melanoma develop. Understanding what causes melanoma and whether you’re at high risk of developing the disease can help you prevent it or detect it early when it is easiest to treat and cure.
However, it is clear that excessive sun exposure, especially severe blistering sunburns early in life, can promote melanoma development. There is evidence that ultraviolet radiation used in indoor tanning equipment may cause melanoma. The risk for developing melanoma may also be inherited.
Anyone can get melanoma, but fair-skinned sun-sensitive people are at a higher risk. Since utraviolet radiation from the sun is a major culprit, people who tan poorly, or burn easily are at the greatest risk.
In addition to excessive sun exposure throughout life, people with many moles are at an increased risk to develop melanoma. The average person has around 30 moles, and most are without significance; however, people with more than 50 moles are at a greater risk. In addition to the number of moles, some people have moles that are unusual and irregular looking. These moles (nevi) are known as dysplastic or atypical moles. People with atypical moles are at increased risk of developing melanoma. Melanoma also runs in families. If a relative such as a parent, aunt or uncle had melanoma, other blood relatives are at an increased risk for melanoma.
The following factors help to identify those at risk for melanoma:
Anyone can develop melanoma, but people with one or more of the risk factors are more likely to do so. Annual skin examinations by a board-certified dermatologist can truly be life saving.
To help you find melanoma and other skin cancers early, dermatologists encourage everyone to learn the following:
The ABCDEs of melanoma
Learn to recognize a possible melanoma by learning these 5 warning signs.
How to perform a skin self-exam
Watch this short video to learn how to check your own skin for signs of melanoma and other skin cancers.