

We recommend annual skin cancer screenings for almost everyone. Essentially all skin cancer can be cured if detected early, and an annual skin cancer screening is the best way to find them at this early stage. Patients with a skin cancer history usually require screening every 3 to 6 months. Skin cancer screenings are truly life saving! Don’t be shy—make your appointment today! Contact us today to schedule an appointment.
Dr. Robinson offers a full 20-30 minute thorough skin exam. You'll be given a gown and asked to take off everything but your undergarments. The gown and undergarments can be moved in ways to keep areas of your body covered during the exam and to protect your privacy. Your appointment will involve a thorough examination of your skin — from the top of your scalp to the bottoms of your feet — by a board-certified dermatologist. Remove any nail polish, this will allow us to fully examine your fingers, nails, and nail beds. We will look for suspicious spots that could be cancerous.
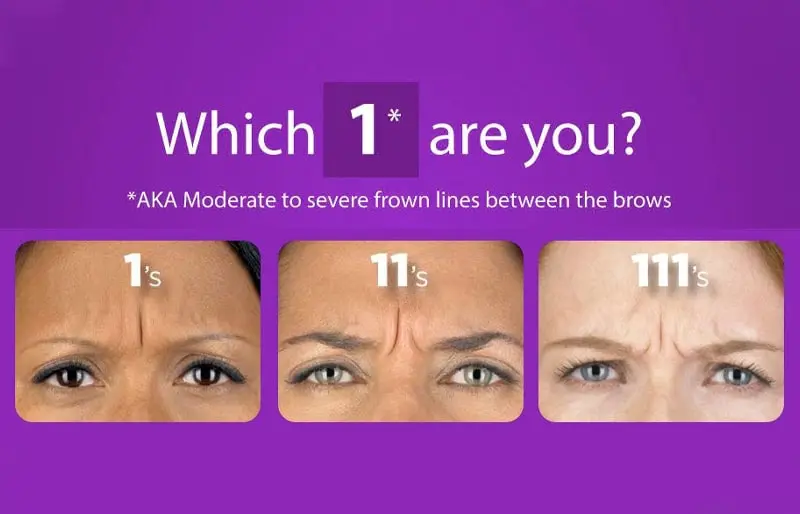
After years of sun, squinting, laughing, frowning, smoking, and worrying, the skin around the eyes and on the forehead will often develop deep lines and wrinkles called “expression lines.” A frequent concern is that they often make you look older, tired, or stressed. Until recently, these advanced furrows have been difficult to treat. Now, by utilizing this FDA approved temporary muscle-relaxing agent, you can reduce "permanent expression lines". Botox® & Xeomin® are “neuromodulators,” an extremely popular agent used to treat the lines of motion that are accentuated with facial movement and expression. It is one of our favorite procedures to perform because of the extremely high patient satisfaction rate, and a great place to start if you are considering a cosmetic procedure for the first time.
If you want to prevent the earliest fine lines from becoming full-blown wrinkles, preventative Botox can be the solution. Botox® is approved for patients who are 18 years and older and most experts agree that patients in their mid to late 20s and early 30s are at a good age for preventative Botox treatment.
With a very fine needle, BOTOX is painlessly injected into the specific muscle that is contracting and causing the lines and wrinkles on the face. No anesthetic is required. Treatment is effective, safe, and takes approximately 10 minutes. Immediately following treatment you may resume regular activities.
The effects usually last 3 to 4 months, and fade away gradually. Following several treatments, the results may last 4 to 8 months or longer. BOTOX® offers extended relief over the course of long-term treatment.
Side effects of BOTOX®, if any, are usually mild and temporary. Botulinum toxins contain proteins, which in some circumstances may be naturally safeguarded against by the body?s ability to produce antibodies. If antibodies are formed, the therapy will generate a lesser response. Temporary bruising, mild pain and swelling are sometimes experienced, though these symptoms resolve on their own within 3 to 5 days. In rare cases, there can be a slight drooping of an eyelid or asymmetry of expression. If this should happen return to our office.
The do’s:
The don’ts :
Typically, the effect of BOTOX® is visible within 5 -7 days. Maximum benefits are reached between 10 to 14 days. Once the muscle becomes dormant and the skin softens, you will have a more relaxed and youthful appearance. BOTOX® treatments are not a substitute for the results achieved with a facelift. The optimum appearance may be achieved with BOTOX® therapy in conjunction with a facelift, dermal fillers, laser resurfacing, and skin rejuvenation.
BOTOX® is a therapeutic muscle-relaxing agent derived from the bacterium, Clostridium Botulinum. For over a decade ophthalmologists have applied BOTOX® for it's original intention, the treatment of blepharospasm. Physicians have utilized BOTOX® for years as a cosmetic treatment to correct visible signs of stress and aging.
The contractions and movements of the facial muscles are controlled by signals from the brain. BOTOX simple prevents the muscle from allowing responses to these messages. As a result, the muscle relaxes and the overlying skin remains unwrinkled and smooth.
Botox injections have been FDA approved to treat excessive sweating. In the skin, Botox selectively turns off the sweat glands resulting in a normal appearance without wetness. Treatment is performed during an outpatient visit and no recuperative time or special care is needed afterward.



Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.




Wrinkles are caused by the natural aging process, expressions made by muscles and sun damage. Using Sunscreen daily is the Holy Grail Anti-Aging product. Today there are many treatments available to help reduce fine lines and wrinkles on the skin. For deeper creases, a person may require more aggressive technique. With the latest treatments such as Botox, Fillers, Ultherapy, TempSure, and Fraxel laser skin resurfacing, wrinkles can appear less noticeable and even be prevented. These treatments are easy in office procedures that require little to no social downtime. The results can be immediate or seen in just a few weeks. Say "Good-bye" to wrinkles and fine lines and hello to beautiful, younger, smoother looking skin.
Cosmetic Consultation Reimbursement policy offered to all patients. Come discuss your needs and goals with Dr. Robinson and the office visit cost will be applied to future costs for the discussed procedure. Procedure must be completed within 30 days of your consult visit.
Warts are non-cancerous skin growths caused by a viral infection in the top layer of the skin. Viruses that cause warts are called human papillomavirus (HPV). The types of HPV that cause common warts, plantar warts, or flat warts are usually different from the types of HPV that cause genital warts. A vaccine is available to help protect against the types of HPV that cause genital warts (and increase a person's risk of certain types of cancer).
There are several different kinds of warts including:
Common warts usually grow on the fingers, around the nails and on the backs of the hands. They are more common where skin has been broken, for example where fingernails are bitten or hangnails picked. These are often called "seed" warts because the blood vessels to the wart produce black dots that look like seeds.
Foot warts usually appear on the soles (plantar area) of the feet and are called plantar warts. When plantar warts grow in clusters they are known as mosaic warts. Most plantar warts do not stick up above the surface like common warts because the pressure of walking flattens them and pushes them back into the skin. Like common warts, these warts may have black dots. Plantar warts are uncomfortable and painful, feeling like a stone in the shoe.
Flat warts appear as small, smooth usually skin colored, pink or brown bumps on the skin. Common places for flat warts are the face, top of the hands, top of the feet, arms, and legs.
Genital warts (warts in the genital area, also called "condyloma acuminatum"
To prevent warts from spreading, dermatologists recommend the following:
While you can often clear a wart at home, some warts can be stubborn. If the person has a weakened immune system, it can be difficult to get rid of warts. Sometimes, what looks like a wart turns out to be a callus or another type of growth.
A board-certified dermatologist can help by:
Sometimes, warts can be stubborn, so they don’t clear with treatment that you can buy without a prescription. A dermatologist can create an effective treatment plan.
Vitiligo is a skin condition resulting from the loss of pigment which produces white patches. Any part of the body may be affected. Usually both sides of the body are affected. Common areas of involvement are the face, lips, hands, arms, legs, and genital areas.
Vitiligo affects one or two of every 100 people. About half the people who develop it do so before the age of 20; about 1/5 have a family member with this condition. It may be an autoimmune process (the body makes antibodies to its own pigment cells). Most people with vitiligo are in good general health, although vitiligo may occur with other autoimmune diseases such as thyroid disease
Melanin, the pigment that determines color of skin, hair, and eyes, is produced in cells called melanocytes. If these cells die or cannot form melanin, the skin becomes lighter or completely white
Typical vitiligo shows areas of milky-white skin. However, the degree of pigment loss can vary within each vitiligo patch. There may be different shades of pigment in a patch, or a border of darker skin may circle an area of light skin.
Vitiligo often begins with a rapid loss of pigment. This may continue until, for unknown reasons, the process stops. Cycles of pigment loss, followed by times where the pigment doesn't change, may continue indefinitely.
It is rare for skin pigment in vitiligo patients to return on its own. Some people who believe they no longer have vitiligo actually have lost all their pigment and no longer have patches of contrasting skin color. Although their skin is all one color, they still have vitiligo.
The course and severity of pigment loss differ with each person. Light-skinned people usually notice the contrast between areas of vitiligo and suntanned skin in the summer. Year round, vitiligo is more obvious on people with darker skin. Individuals with severe cases can lose pigment all over the body. There is no way to predict how much pigment an individual will lose.
Sometimes the best treatment for vitiligo is no treatment at all. In fair-skinned individuals, avoiding tanning of normal skin can make areas of vitiligo almost unnoticeable because the (no pigment) white skin, of vitiligo has no natural protection from sun. These areas are easily sunburned, and people with vitiligo have an increased risk to skin cancer. A sunscreen with a SPF of at least 30 should be used on all areas of vitiligo not covered by clothing. Avoid the sun when it is most intense to avoid burns.
Disguising vitiligo with make-up, self-tanning compounds or dyes is a safe, easy way to make it less noticeable. Waterproof cosmetics to match almost all skin colors are available. Stains that dye the skin can be used to color the white patches to more closely match normal skin color. These stains gradually wear off. Self-tanning compounds contain a chemical called dihydroxyacetone that does not need melanocytes to make the skin a tan color. The color from self-tanning creams also slowly wears off. None of these change the disease, but they can improve appearance. Micropigmentation tatooing of small areas may be helpful.
If sunscreens and cover-ups are not satisfactory, your doctor may recommend other treatment. Treatment can be aimed at returning normal pigment (repigmentation) or destroying remaining pigment (depigmentation). None of the repigmentation methods are permanent cures.
Aggressive treatment is generally not used in children. Sunscreen and cover-up measures are usually the best treatments. Topical corticosteroids can also be used, but must be monitored. PUVA, an ulta-violet therapy, is usually not recommended until after age 12, and then the risks and benefits of this treatment must be carefully weighed.
Topical Corticosteroids — Creams containing corticosteroid compounds can be effective in returning pigment to small areas of vitiligo. These can be used along with other treatments. These agents can thin the skin or even cause stretch marks in certain areas. They should be used under your dermatologist's care.
PUVA is a form of repigmentation therapy where a type of medication known as psoralen is used. This chemical makes the skin very sensitive to light. Then the skin is treated with a special type of ultraviolet light call UVA. Sometimes, when vitiligo is limited to a few small areas, psoralens can be applied to the vitiligo areas before UVA treatments. Usually, however, psoralens are given in pill form. Treatment with PUVA has a 50 to 70% chance of returning color on the face, trunk, and upper arms and upper legs. Hands and feet respond very poorly. Usually at least a year of twice weekly treatments are required. PUVA must be given under close supervision by your dermatologist. Side effects of PUVA include sunburn-type reactions. When used long-term, freckling of the skin may result and there is an increased risk of skin cancer. Because psoralens also make the eyes more sensitive to light, UVA blocking eyeglasses must be worn from the time of exposure to psoralen until sunset that day to prevent an increased risk of cataracts. PUVA is not usually used in children under the age of 12, in pregnant or breast feeding women, or in individuals with certain medical conditions.
This is a form of phototherapy that requires the skin to be treated two, sometimes three, times a week for a few months. At this time this form of treatment is not widely available. It may be especially useful in treating children with vitiligo.
Transfer of skin from normal to white areas is a treatment available only in certain areas of the country and is useful for only a small group of vitiligo patients. It does not generally result in total return of pigment in treated areas.
Other treatment options include a new topical class of drugs called immunomodulators. Due to their safety profile they may be useful in treating eyelids and children. Excimer lasers may be tried as well.
For some patients with extensive involvement, the most practical treatment for vitiligo is to remove remaining pigment from normal skin and make the whole body an even white color. This is done with a chemical called monobenzylether of hydroquinone. This therapy takes about a year to complete. The pigment removal is permanent.
At this time, the exact cause of vitiligo is not known, however, there may be an inherited component. Although treatment is available, there is no single cure. Research is ongoing in vitiligo and it is hoped that new treatments will be developed.
Time To Smile Again ... A venous lake is a benign, soft, compressible blue bump usually found on or around the lips caused by a dilated vein. While it is benign it can be cosmetically unsightly. With the use of the Nd:YAG laser a venous lake can be treated within seconds and resolved without scarring.
What To Expect:
FAQ's:
Is It Safe? The Nd:YAG laser is clinically proven to be both safe and effective.
How Does It Work? Treatments target the blood in the venous Lake lesion, causing it to regress.
Is The Treatment Suitable For Me? This procedure can be used on all skin types and treatment is suitable for most people. However, prior to treatment please review our cosmetic reimbursement policy.
Urticaria, also known as hives, are localized, pale, itchy, pink wheals (swellings) that can burn or sting. They may occur singularly or in groups on any part of the skin. They are part of an allergic reaction and are very common. Approximately 10-20 percent of the population will have at least one episode in their lifetime. Most episodes of hives disappear quickly in a few days to a few weeks. Occasionally, a person will have them for many months or years. New hives may develop as old ones fade. Hives can vary in size from as small as a pencil eraser to as large as a dinner plate, and may join to form even larger swellings.
Hives are produced by blood plasma leaking through tiny gaps between the cell lining small blood vessels in the skin. Histamine is a chemical released from cells in the skin called mast cells; which lie along blood vessels. Allergic reactions, chemicals in foods, or medications may cause hives; sometimes it is impossible to find out the cause. When hives form around the eyes, lips, or genitals, the tissue may swell excessively. Although frightening, the swelling usually goes away in less than 24 hours. Severe cases of hives may cause difficulty in breathing or swallowing and emergency room care is required.
Acute urticaria lasts less than six weeks. An underlying cause can be frequently identified and eliminated. The most common causes for acute urticaria are foods, drugs, or infections. Insect bites, internal diseases, pressure, cold, or sunlight also may be responsible.
The most common foods that cause urticaria are: nuts, chocolate, shellfish, tomatoes, eggs, berries, and milk. Fresh foods cause hives more often than cooked foods. Food additives and preservatives may also cause hives.
Hives may appear within minutes to several hours after eating, depending upon the site within the digestive tract where the food is absorbed.
Almost any medication -- prescription or over-the-counter -- can cause hives. Antibiotics, pain medications, sedatives, tranquilizers, diuretics (water pills), diet supplements, antacids, arthritis medication, vitamins, herbal supplements, eye and eardrops, laxatives, vaginal douches, or any other non-prescription item can be a potential cause of urticaria. It is important to inform the dermatologist of ALL prescription and over-the-counter medications being used to help find the cause of the hives.
Many infections can cause urticaria. Viral upper-respiratory tract infections (colds) are a comon cause in children. Other viruses, including hepatitis and a number of bacterial and fungal infections, may cause urticaria.
Chronic urticaria lasts more than six weeks. The cause of chronic urticaria is more difficult to identify and is found only in a small percentage of patients. The dermatologist reviews a patient's medical history, asks extensive questions, and conducts a thorough physical examination. Testing, such as blood work or a biopsy, may be necessary.
Physical urticaria may be caused by sunlight, heat, cold, water, pressure, vibration, or exercise. Solar urticaria forms within minutes of sun exposure and typically fades within one to two hours. Cold urticaria appears when the skin is warmed after exposure to cold. Urticaria, which forms in response to the cold or the water when swimming, for example, can produce wheezing, flushing, generalized hives, and fainting.
Dermatographic urticaria forms after firmly stroking or scratching the skin, and can often occur with other forms of urticaria. It affects about five percent of the population. Most people with this condition are otherwise healthy. Dermatographism may last for months or even years.
The best treatment for urticaria is to find and eliminate the cause whenever possible. Antihistamines are prescribed to provide relief and work best if taken on a regular schedule to prevent hives from forming. There are many antihistamines available. No one antihistamine works for everyone. The dermatologist may use combinations to control the urticaria. In severe cases, an injection of epinephrine (adrenalin) may be needed. Cortisone may also bring dramatic relief, but its use must be limited to short periods of time.
Tinea versicolor is a common skin condition due to overgrowth of a skin surface yeast. This overgrowth results in uneven skin color and scaling that can be unsightly and sometimes itch. The yeast normally lives in the pores of the skin and thrives in oily areas such as the neck, upper chest, and back. Tinea versicolor has small, scaly white-to-pink or tan-to-dark spots which can be scattered over the upper arms, chest and back. They may sometimes appear on the neck and the face. On light skin, Tinea versicolor may be faint or can appear as tan-to-pink spots, while on dark skin Tinea versicolor may be light or dark. The fungus grows slowly and prevents the skin from tanning normally. As the rest of the skin tans in the sun, the pale spots, which are affected by the yeast, become more noticeable, especially on dark skin.
Tinea versicolor has small, scaly white-to-pink or tan-to-dark spots which can be scattered over the upper arms, chest and back. They may sometimes appear on the neck and the face. On light skin, Tinea versicolor may be faint or can appear as tan-to-pink spots, while on dark skin Tinea Versicolor may be light or dark. The fungus grows slowly and prevents the skin from tanning normally.
Tinea Versicolor usually produces few symptoms. Occasionally, there is some slight itching that is more intense when a person gets hot.
Most people get tinea versicolor when they are teenagers or young adults. It is rare in the elderly and children, except in tropical climates where it can occur at any age. Both dark and light skinned people are equally prone to its development. People with oily skin may be more susceptible than those with naturally dry skin.
The yeast is normally present in small numbers on everyone's skin. Anyone can develop an overgrowth of yeast. During the summer months when the temperature and humidity are high, the yeast can increase. The excess yeast on the skin prevents the normal pigmentation process, resulting in light and dark spots. In tropical countries with continuous high heat and high humidity, people can have these spots year round. In other climates, the spots generally fade in the cooler and drier months of the year. Why some people get tinea versicolor and others do not is unclear.
In tropical countries with continuous high heat and high humidity, people can have these spots year round. In other climates, the spots generally fade in the cooler and drier months of the year.
Although the light or dark colored spots can resemble other skin conditions, tinea versicolor can be easily recognized by a dermatologist. In most cases, the appearance of the skin is diagnostic, but a simple examination of the fine scales scraped from the skin can confirm the diagnosis. Scales are lightly scraped onto a slide and examined under a microscope for the presence of the yeast. A special light may help to make the diagnosis by showing a yellow green color where the skin is affected.
Tinea versicolor is treated with topical or oral medications. Topical treatment includes special cleansers including some shampoos, creams, or lotions applied directly to the skin.
Several oral medications have been used successfully to treat tinea versicolor. Because of possible side effects, or interactions with other medications, the use of these prescription medicines should be supervised by a dermatologist. After any form of treatment, the uneven color of the skin may remain for several months after the yeast has been eliminated until the skin repigments normally.
Tinea versicolor may recur. Special cleansers may decrease episodes when used once or twice a month, especially during warm humid months of the year.
Each patient is treated by the dermatologist according to the severity and location of the disease, the climate, and the desire of the patient. It's important to remember that the yeast is easy to kill, but it can take weeks or months for the skin to regain its normal color.
Telangectasias (commonly known as spider veins) are dilated or broken blood vessels located near the surface of the skin. They often occur on the face and particularly on the sides of the nose. They often look like small red or pink lines, which temporarily whiten when pressed.
Some Symptoms Of Spider Veins Include:
Common Causes of Spider Veins
Spider veins are generally caused by weak or damaged valves. The following causes can contribute to weaker blood flow in certain areas of your body.
Treatment(s):
Thankfully, laser therapy is safe and efficacious treatment. It is an easy in-office treatment that can be performed during ones lunch break. In 10 minutes those red lines are gone and you can go right back to work. No wound care or dressings needed.
Sclerotherapy is also a treatment option. A special solution is injected directly into the affected veins, forcing the veins to close and the blood to redirect into healthier veins. The old vein turns into scar tissue that your body will eventually absorb, causing it to fade.
Lately, the decision to obtain a tattoo has become increasingly popular, and so has the decision to remove them! DON'T REGRET IT ... REMOVE IT! An estimated 20 million Americans have tattoos, and many of them now feel that having a tattoo does not fit their image. Those remorseful about their tattoos are consulting with cosmetic laser physicians to determine if the removal of their tattoo is possible. Today's advanced laser technology provides the means for tattoo removal safely and quickly and, in most cases, without leaving a scar. Complete removal of all types of tattoos, on all skin types, in up to half the treatments.
Cosmetic medical lasers designed to eradicate tattoos range from a single wavelength of light to a broad spectrum of light, the varieties of which are intended to obliterate the ink in the tattoo without damaging the skin. Certain colors of light are absorbed by specific corresponding colors of the tattoo ink. The light energy vaporizes or fragments the ink particles. Your body then absorbs these ink fragments naturally and the color fades over the next couple of weeks. This treatment is very similar to methods used for years to treat birthmarks.
Ask us about our "Cosmetic Consultation Reimbursement" policy offered to all patients. Come discuss your needs and goals with Dr. Robinson and the office visit cost will be applied to future costs for the discussed procedure. Procedure must be completed within 30 days of your consult visit.



