

Alopecia areata (AA) causes hair loss in small, round patches that may go away on their own, or may last for many years. Nearly 2% of the U.S. population (about four million people) will develop AA in their lifetime. Some people with AA (about 5%) may lose all scalp hair (alopecia totalis) or all scalp and body hair (alopecia universalis). It is an autoimmune disease, in which for unknown reasons your immune system attacks your own hair follicles, (where the hair grows from), resulting in damage that leads to hair loss anywhere on the body. Typically, it affects small patches of hair so, it may go completely unnoticed. However, more patches of hair loss could develop close together, making it more noticeable.
AA occurs world-wide in both genders and in every ethnic group. Children and young adults are most frequently affected, but persons of all ages are susceptible. One in five persons with AA has a family member who also has the disease.
AA usually begins with one or more small, round, coin-size, bare patches. It is most common on the scalp, but can involve any hair-bearing site on the body including eyebrows, eyelashes, and beards. Hair may fall out and regrow with the possibility of full hair regrowth always present. AA usually has no associated symptoms, but there may be minor discomfort or itching prior to developing a new patch. Nails may have tiny pinpoint dents, ridges, become brittle and may, in rare instances, become distorted.

AA is not contagious. It is an autoimmune disease in which the body's immune system attacks itself, in this case, the hair follicles. The cause is not known. A person's particular genetic makeup combined with other factors triggers AA.
The main types are:
Alopecia areata: Alopecia is the medical term for bald. Areata means patchy. This patchy baldness can develop anywhere on the body, including the scalp, beard area, eyebrows, eyelashes, armpits, inside your nose, or ears.
Alopecia totalis: The person loses all hair on the scalp, so the scalp is completely bald.
Alopecia universalis: The person loses all hair, leaving the entire body hairless. This is rare.
Although your dermatologist may know by examining your scalp that you have AA, occasionally, a scalp biopsy is helpful in confirming the diagnosis.
Because there are so many reasons for hair loss, testing is sometimes necessary to make sure alopecia areata is the cause of your hair loss.
A blood test can look for other diseases caused by the immune system. Sometimes, other tests are necessary.
AA is not a symptom of a serious disease and usually occurs in otherwise healthy individuals. Persons with AA may have a higher risk of atopic eczema, asthma, and nasal allergies, as well as other autoimmune diseases such as thyroid disease (Hashimoto's thyroiditis), and vitiligo. Family members may also have atopic eczema, asthma, nasal allergies, or autoimmune diseases (i.e. insulin-dependent diabetes, rheumatoid arthritis, thyroid disease, or systemic lupus erythematosus).

Yes, it is likely that the hair may regrow, but it may fall out again. The course of the disease varies from person to person, and no one can predict when the hair might regrow or fall out again. This unpredictability of AA, and the lack of control over it, makes this condition frustrating. Some people lose a few patches of hair, the hair regrows, and the condition never returns. Other people continue to lose and regrow hair for many years. The potential for full regrowth is always there, even in people who lose all the hair on their scalp and body (alopecia totalis/universalis). Hair could regrow white or fine, but the original hair color and texture may return later.
The good news is that many causes of hair loss can be managed when caught early and further loss can usually be slowed or prevented.
Corticosteroids are anti-inflammatory drugs that suppress the immune system. They can be given as injections into the areas of hair loss, rubbed topically into affected areas or taken orally as pills.
Oral Minoxidil is by prescription only. Dermatologists began using low-dose oral minoxidil for hair loss after noticing the side effects of the high-dose version of the drug used to treat high blood pressure increased hair growth. The efficacy of 5mg oral minoxidil for men with androgenetic alopecia was tested. Researchers concluded that 43% of the patients had excellent results in hair growth. Typically, people prefer oral to topical. They find it easier and more convenient to take the medication orally, may be able to save money with an oral minoxidil prescription and prefer not to have residue on their hair.
Topical Minoxidil 5% Solution aka Rogaine solution or foam is available over the counter. Effectiveness of topical Minoxidil works for about 2 out of 3 men. It's most effective if you're under age 40 and have only recently started to lose your hair. How to use it: Twice a day, when your hair is dry, apply minoxidil on your scalp where the hair has started to thin. Minoxidil can help maintain the regrowth after you stop applying the corticosteroid. It has few side effects, so it’s considered a good option for children. New hair growth may appear in about 12 weeks.
PRP (platelet-rich plasma) therapy for hair loss is a three-step medical treatment in which a person’s blood is drawn, processed, and then injected into the scalp.
PRP injections trigger natural hair growth and maintain it by increasing blood supply to the hair follicle and increasing the thickness of the hair shaft. Sometimes this approach is combined with other hair loss procedures or medications.
PRP therapy is a three-step process. Most PRP therapy requires three treatments 4–6 weeks apart.
Maintenance treatments are required every 4–6 months.
Your blood is drawn — typically from your arm — and put into a centrifuge (a machine that spins rapidly to separate fluids of different densities).
After about 10 minutes in the centrifuge, your blood will have separated into in three layers:
The platelet-rich plasma is drawn up into a syringe and then injected into areas of the scalp that need increased hair growth.
There hasn’t been enough research to prove whether PRP is effective. It’s also unclear for whom — and under what circumstances — it’s most effective.
Wigs, caps, hats, or scarves are important options. Wearing a head covering does not interfere with hair regrowth. This may be a good choice for people with extensive scalp hair loss who do not have enough hair to cover it.
The emotional aspects of living with hair loss can be challenging, especially in a society that regards hair as a sign of youth and good health. It is reassuring that alopecia areata does not affect general health, and should not interfere with your ability to achieve all of your life goals at school, in sports, in your career, and in raising a family.
The National Alopecia Areata Foundation, the NAAF, is a great resource for support, treatment & education.
Schedule an appointment to see which treatment or combination of treatments is the best choice for you.
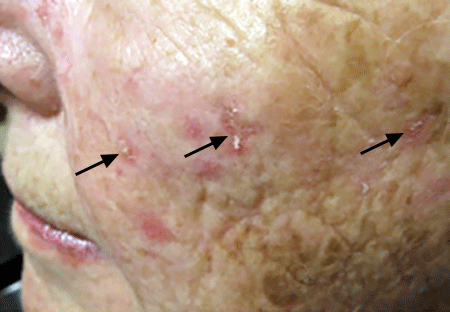
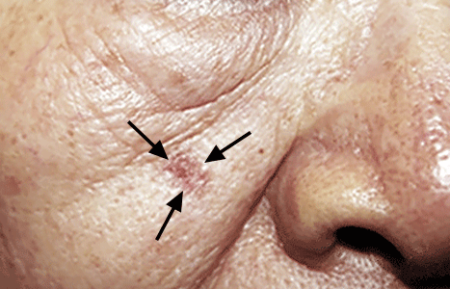
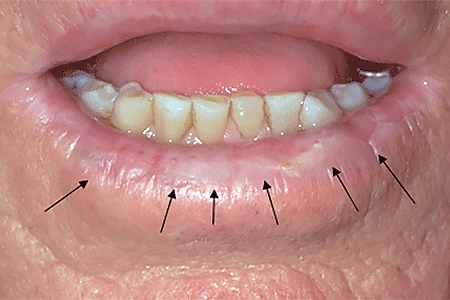
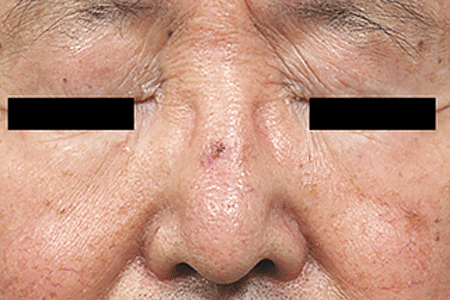
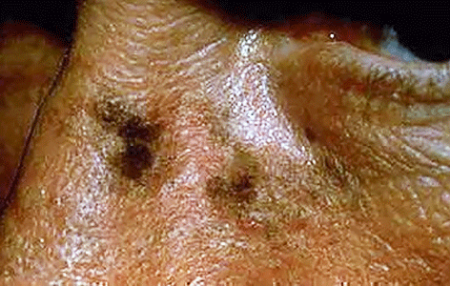
An actinic keratosis, is a rough, scaly patch on the skin that develops from years of sun exposure. It's often found on the face, lips, ears, forearms, scalp, neck or back of the hands. These represent pre-cancerous growths that can become skin cancer if left untreated.
If you find a spot or growth on your skin that you think could be an actinic keratosis (AK), it’s time for a thorough skin exam. Should you have an AK, an accurate diagnosis and treatment can:
Most people who have AKs (or think they may have an AK) see a dermatologist. This is actually one of the most common conditions that dermatologists diagnose and treat.
When you see a board-certified dermatologist about AKs, your dermatologist will:
If you have one or more AKs on your skin, a board-certified dermatologist can often diagnose you by looking carefully at your skin. While examining your skin, your dermatologist will also look for signs of skin cancer. People who have skin that’s been badly damaged by ultraviolet (UV) light develop AKs and have a higher risk of getting skin cancer.
If you have one or more AKs, your dermatologist will talk with you about whether to treat these precancerous skin growths. Usually, treatment is recommended.
For a few people, a dermatologist may recommend frequent skin exams rather than treatment. Skin exams are recommended for patients who are frail and may find it hard to tolerate treatment. To be effective, treatment must destroy the AKs. When this happens, your skin will feel raw. It may be red and swollen for a brief time.
The treatment that is right for you depends on several considerations, including:
If you have one or a few AKs, a procedure that your dermatologist can perform during an appointment may be the preferred treatment.
You can often complete treatment in 1 or 2 office visits. The procedures that dermatologists use to treat AKs include:
Some people develop a few AKs, which can often be cleared with treatment.
If you have many AKs, it’s a good idea to be under a dermatologist’s care. Your skin has been severely damaged by UV light, so it’s likely you’ll continue get new AKs. You may also develop skin cancer. Your dermatologist can watch for signs of new AKs and skin cancer. When found early and treated, skin cancer is highly treatable.
Your dermatologist will tell you how often to return for check-ups. Some people need a check-up once or twice a year. If you have a weakened immune system or a rare condition that greatly increases your risk of developing AKs and skin cancer, you may need to see your dermatologist every 8 to 12 weeks.
Keep every appointment. If skin cancer develops, the sooner it is found and treated, the better your outcome.
Self-care also plays a key role in your outcome. The right self-care can help to prevent new AKs and skin cancer.


Acne is a skin condition which has plugged pores (blackheads and whiteheads), inflamed pimples (pustules), and deeper lumps (nodules). Acne occurs on the face, as well as the neck, chest, back, shoulders, and upper arms. Although most teenagers get some form of acne, adults in their 20's, 30's, 40's, or even older, can develop acne. Often, acne clears up after several years, even without treatment. Acne can be disfiguring and upsetting to the patient. Untreated acne can leave permanent scars; these may be treated by your dermatologist in the future. To avoid acne scarring, treating acne is important.
Acne is not caused by dirt. Testosterone, a hormone which is present in both males and females, increases during adolescence (puberty). It stimulates the sebaceous glands of the skin to enlarge, produce oil, and plug the pores. Whiteheads (closed comedones), blackheads (open comedones), and pimples (pustules) are present in teenage acne.
Early acne occurs before the first period and is called prepubertal acne. When acne is severe and forms deep "pus-filled" lumps, it is called cystic acne. This may be more common in males. Adult acne develops later in life and may be related to hormones, childbirth, menopause, or stopping the pill. Adult women may be treated at the period and at ovulation when acne is especially severe, or throughout the entire cycle. Adult acne is not rosacea, a disease in which blackheads and whiteheads do not occur.
Acne has nothing to do with not washing your face. However, it is best to wash your face with a mild cleanser and warm water daily. Washing too often or too vigorously may actually make your acne worse.
Acne is not caused by foods. However, if certain foods seem to make your acne worse, try to avoid them.
Wear as little cosmetics as possible. Oil-free, water-based moisturizers and make-up should be used. Choose products that are "non-comedogenic" (should not cause whiteheads or blackheads) or "non-acnegenic" (should not cause acne). Remove your cosmetics every night with mild soap or gentle cleanser and water.
A flesh-tinted acne lotion containing acne medications can safely hide blemishes. Loose powder in combination with an oil-free foundation is also good for cover-up.
Shield your face when applying sprays and gels on your hair.
Control of acne is an ongoing process. All acne treatments work by preventing new acne breakouts. Existing blemishes must heal on their own, and therefore, improvement takes time. If your acne has not improved within two to three months, your treatment may need to be changed. The treatment your dermatologist recommends will vary according to the type of acne.
Occasionally, an acne-like rash can be due to another cause such as make-up or lotions, or from oral medication. It is important to help your dermatologist by providing an updated history of what you are using on your skin or taking internally.
Many non-prescription acne lotions and creams help mild cases of acne. However, many will also make your skin dry. Follow instructions carefully.
Re-think your skin health. Hydrafacial MD, - * Acne Facial, is highly effective for anyone suffering from oily and/or acne-prone skin. It visibly reduces redness, enlarged pores, hyperpigmentation, utilizing LED blue light killing acne causing bacteria. HydraFacial MD - Hydradermabrasion is the latest, non-invasive, "gentle" skin resurfacing and complexion treatment. The immediate, noticeable, long lasting results are achieved with zero downtime and without any discomfort. You can return to school, work, social life, or exercise right after your procedure. HydraFacial MD uses a uniquely shaped spiral tip and patented vortex fusing technology to gently cleanse, exfoliate, and extract, removing impurities and dead skin cells while hydrating the skin and adding antioxidant protection simultaneously.
Acne scars no longer have to be lived with forever. Often occurring on the face, back and chest these scars can now be treated with a variety of lasers (Fraxel®, V-Beam), subcission or chemical peels. These treatments require no social downtime and can be performed on all skin colors.
A surgical excision is an in-office procedure in which a skin lesion is removed by a dermatologic surgeon. This technique involves the use of local numbing medicine which is injected into and around the target area and followed by sharp dissection of the lesion from surrounding normal tissue. The most common scenarios for utilization of this technique include: treatment of skin cancers, atypical or suspicious moles (nevi), and cysts.
Cysts may remain asymptomatic, but if they continue to grow or become painful surgical excision is the treatment of choice. The cyst consists of a wall that makes the contents. To insure that the cyst does not return, it is best to completely excise it, including the wall, to prevent its recurrence.
Moles often become more raised over time. Occasionally they become irritated or are cut when shaving. A shave excision removes the raised portion of the mole. As a general rule, a complete excision is only performed if a mole is changing or when a complete excision will yield a better cosmetic result. Either of these treatments is performed under local anesthesia in our office. The shave excision takes less than a minute and a complete excision under a half hour. The functional and cosmetic results are excellent.
This option is typically for scars that are deeply pitted, raised, or for older surgical scars that did not heal properly. The scar tissue is removed, followed by careful stitching of the skin to leave a much smaller, thinner scar line or to change the scars shape and/or direction so it is less obvious.
Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
You're more likely to get Lyme disease if you live or spend time in grassy and heavily wooded areas where ticks carrying Lyme disease thrive. It's important to take common-sense precautions in tick-infested areas.
Where you live or vacation can affect your chances of getting Lyme disease. So can your profession and the outdoor activities you enjoy. The most common risk factors for Lyme disease include:


A small, red bump, similar to the bump of a mosquito bite, often appears at the site of a tick bite or tick removal and resolves over a few days. This normal occurrence doesn't indicate Lyme disease.
However, these signs and symptoms can occur within a month after you've been infected:

If untreated, new signs and symptoms of Lyme infection might appear in the following weeks to months. These include:
Several weeks after infection, some people develop:
If you've been bitten by a tick and have symptoms, only a minority of tick bites lead to Lyme disease. The longer the tick remains attached to your skin, the greater your risk of getting the disease. Lyme infection is unlikely if the tick is attached for less than 36 to 48 hours.
If you think you've been bitten and have signs and symptoms of Lyme disease — particularly if you live in an area where Lyme disease is common — contact your doctor. Treatment for Lyme disease is more effective if begun early.
Visit your doctor even if signs and symptoms disappear — the absence of symptoms doesn't mean the disease is gone. Untreated, Lyme disease can spread to other parts of your body for several months to years after infection, causing arthritis and nervous system problems. Ticks can also transmit other illnesses, such as babesiosis and Colorado tick fever.
The best way to prevent Lyme disease is to avoid areas where deer ticks live, especially wooded, bushy areas with long grass. You can decrease your risk of getting Lyme disease with some simple precautions:
What is intralesional steroid injection used for?
Intralesional Steroid Injections, or Intralesional Kenalog is a common treatment used in dermatology & are a standard treatment for many skin diseases including: acne lesions, cysts, alopecia (bald spots) hair loss, eczema, abundant scar tissue (keloids, hypertrophic scars), psoriasis, lichen simplex chronicus, skin lupus, granuloma annulare, and more. Intralesional injections are extremely helpful, as they are able to bypass the outer defensive layers of the skin to reach an area that will make the greatest impact on your condition. It is common for a patient to need multiple injections, as different cases vary in severity. The goal of these injections is ideal for quick healing to reduce the inflammation within the skin, and relive pain and discomfort as well as improving the appearance. This treatment is usually reserved for tender, swollen acne nodules, or cysts that aren't responding to typical acne therapies. Prompt treatment with intralesional injections can often prevent scarring.
Canthrone is an excellent treatment for warts, molluscum and other growths in the skin. It is painless and therefore preferred by many of our pediatric patients and adults who are adverse to even a little discomfort. It is usually applied with a Q-tip (for children we refer to it as a tickle stick) and then covered with paper tape or a bandaid. Patients are instructed to wash it off between twenty minutes to one hour later. Although several treatments may be required, Canthrone is the kindler and gentler treatment for these ailments.
As the United States declares Monkeypox outbreak a public health emergency, NYC declares a local state of emergency due to the outbreak. The American Academy of Dermatology & The World Health Organization have put together a Task Force to address the growing outbreak of Monkeypox (orthopoxvirus) in the US. Monkeypox is a contagious disease caused by the Monkeypox virus. US Map and case count on the 2020 outbreak here ...
Anyone can get Monkeypox. It is primarily spread through close, physical contact between people. In the current outbreak, the Monkeypox virus is spreading mainly during oral, anal and vaginal sex and other intimate contact, such as rimming, hugging, kissing, biting, cuddling and massage.
Previous outbreak experience elsewhere suggests that the elderly, those with weakened immune systems, pregnant people, and children under 8 years of age may be at heightened risk for severe outcomes. Smallpox vaccine may help protect you against Monkeypox. Although, immunity may wain with age, it is estimated that the smallpox vaccine can be over 80% effective in preventing Monkeypox. Howevver, the vaccine for smallpox was discontinued in 1972 when it was eradicated in the United States. So therefore, anyone who is 49 years of age or younger most likely did not receive a smallpox vaccine.
The best way to protect yourself from Monkeypox is to avoid sex and other intimate contact with multiple or anonymous partners.
If you choose to have sex or other intimate contact, the following can help reduce your risk:
How to Protect Yourself and Others from Monkeypox (PDF)
Most cases are mild. Symptoms usually start within two weeks of exposure, but in some cases they may not appear for up to 21 days. If you have a new, unexplained skin rash or lesion(s)/bump(s) on your skin and you don’t know what caused it and think you may have Monkeypox, it is important to see your dermatologist quickly to prevent exposing more people. Eligible New Yorkers who may have been exposed to Monkeypox can now get vaccinated to stay safe and slow the spread.
Some symptoms include:
A person is contagious until all sores have healed and a new layer of skin has formed, which can take two to four weeks.
If you start experiencing symptoms, isolate at home immediately, ideally stay in a separate area away from other family members and pets and talk to your dermatologist.
The following may increase your risk for severe disease if you are infected: HIV; other conditions that weaken your immune system; and a history of atopic dermatitis or eczema. If you have one of these conditions, it is especially important to see a provider right away, if you have symptoms.
To protect others while you are sick:
Not every rash is Monkeypox. Dr. Robinson can make a diagnosis of Monkeypox by looking at the pattern on the skin and where the rash appears. Please let the office know ahead of your visit that you have a "new unexplained rash or lesions" and think you may have monkeypox. If Dr. Robinson suspects Monkeypox may be the cause of the rash, he will swab the rash and send it to a lab, where a polymerase chain reaction test will be performed.
There is treatment approved for Monkeypox. Most people get better on their own without treatment. However, antiviral medication(s) (TPOXX) may help. Your provider will help you find out if you are eligible for antiviral treatment. They may be able to prescribe medicine and provide information about symptom relief.
Vaccination after possible exposure ... Eligible New Yorkers who may have been recently exposed to Monkeypox can get the JYNNEOS TM vaccine. Vaccine is free and available regardless of immigration status. Information about eligibility for the vaccine and appointments can be found here.
Getting vaccinated after a recent exposure may reduce the chance of you getting Monkeypox and it can reduce the symptoms if you do get it.
People should get two doses, at least four weeks apart.
Information about eligibility for the vaccine clinic and appointments can be found here.
JYNNEOS Vaccine for Monkeypox: Frequently Asked Questions (PDF)
Additionally, here is a link to a letter published in the Journal of the American Academy of Dermatology (JAAD) that explains the symptoms and features of monkeypox. For more information about monkeypox, visit the AAD website.

Molluscum Contagiosum rarely causes pain and will eventually clear on its own if you have a healthy immune system. They may go away without a trace, but this takes time, during which they can spread. On average, the bumps clear in 6-18 months without treatment. Sometimes, this takes longer and they can re-occur.
Avoid spreading molluscum to other parts of your body by:
Until the molluscum bumps go away, take precautions to help prevent spreading the molluscum virus to others. Watch what the American Academy of Dermatology recommends here ... https://youtu.be/klkQ2YcJHaw
Dr. Robinson also recommends:
Dr. Robinson offers these tips and others every day to help his patients feel more comfortable in their own skin.
The best way to protect infants from the sun is to keep them in the shade as much as possible, in addition to dressing them in loose fitting long sleeves, pants, a wide-brimmed hat that shields the face, ears, back of the neck and sunglasses with at least 99% UVA/UVB protection. If you can’t find shade, create your own using an umbrella, canopy, or the hood of a stroller. Make sure they do not get overheated and that they drink plenty of fluids. If your baby is fussy, crying excessively, or has redness on any exposed skin, take him or her indoors.
Minimize sunscreen use on children younger than six months old. However, if shade and adequate clothing are not available, The American Academy of Dermatology (AAD) recommends that all kids — regardless of their skin tone — wear sunscreen with an SPF of 30 or higher that is broad-spectrum and water resistant.
For babies older than 6 months, when outdoors, sunscreen should be applied to all areas of the body, but be careful around the eyes. If your baby rubs sunscreen into their eyes, wipe their eyes and hands clean with a damp cloth. Reapply sunscreen every two hours or immediately after getting out of the water. Sunscreens that use zinc oxide may cause less irritation and/or allergic reactions to their sensitive skin. If a rash develops please call our office.
Other elements of a sun safe strategy include: wearing clothing made with a tight weave. If you are not sure how tight a fabric’s weave is, hold it up to see how much light shines through, the less the better. You can also look for protective clothing labeled with Ultraviolet Protection Factor (UPF) and limiting your sun exposure between 10:00 a.m. and 4:00 p.m. when the UV rays are the strongest. Remember to set a good example by practicing sun safety yourself.
The sun gives energy to all living things on earth, but it can also harm us. Its ultraviolet (UV) rays can damage skin and eyes and cause skin cancer. One-quarter of our lifetimes sun exposure happens during childhood and adolescence. Even one blistering sunburn in childhood or adolescence more than doubles your chances of developing Melanoma later in life. Since children spend a lot of time outdoors, especially in the summer, it's important to protect them from the sun.
Talk with your dermatologist if you have any questions about sun protection for your child.

