


It is important to treat a sunburn as soon as you notice it.
The first thing you should do if you feel you have or are getting a sunburn is get out of the sun, preferably go indoors. Once indoors, these tips can help relieve the discomfort:
If you have fever, chills, headache or any questions about your sunburn please call our office to schedule an appointment. Although it may seem like a temporary condition, sunburn is a result of skin receiving too much exposure from the sun’s ultraviolet (UV) rays and can cause long-lasting damage to the skin. This damage increases a person’s risk for getting skin cancer.
Subcission is a treatment used to correct a type of scar called a valley scar. A valley scar simply means there is a defect in the volume of the skin at the site of the scar. The goal of subcission is to improve this decreased volume. This then allows a depressed scar to regain its smooth appearance. This treatment may be combined with other scar treatments to yield the best cosmetic results.
Squamous cell carcinoma is the second most common cancer of the skin. More than 250,000 new squamous cell carcinomas are diagnosed every year in the United States. Middle-aged and elderly people, especially those with fair complexions and frequent sun exposure, are most likely to be affected.
The cancer develops in the outer layer of the skin (the epithelium). Some squamous cell carcinomas arise from small sandpaper-like lesions called solar (sun) or actinic keratosis. It is possible for squamous cell carcinoma to spread to other areas of the body; therefore, early treatment is important.
Squamous cell carcinomas usually appear as crusted or scaly patches on the skin with a red, inflamed base, a growing tumor, or a non-healing ulcer. They are generally found in sun-exposed areas like the face, neck, arms, scalp, backs of the hands, and ears. The cancer also can occur on the lips, inside the mouth, on the genitalia, or anywhere on the body. Any lesion, especially those that do not heal, grow, bleed, or change in appearance, should be evaluated by a dermatologist.
Ultraviolet light exposure (from the sun or indoor tanning devices) greatly increases the chance of developing skin cancer. Although anyone can get squamous cell carcinoma, people with light skin who sunburn easily are at the highest risk. The chance of developing skin cancer increases with age and a history of severe sunburns as a child. Many less common skin conditions, organ transplantation, chronic skin ulcers, prior x-ray treatment (e.g., for acne in the 1950s), arsenic ingestion, smoking, and toxic exposure to tars and oils can predispose individuals to the development of squamous cell carcinoma.
These skin cancers are usually locally destructive. If left untreated, squamous cell carcinoma can destroy much of the tissue surrounding the tumor and may result in the loss of a nose or ear, for example. Aggressive types of squamous cell carcinomas, especially those on the lips and ears, or untreated cancers, can spread to the lymph nodes and other organs resulting in approximately 2,500 deaths each year in the United States.
A skin biopsy for microscopic examination may be done to confirm the diagnosis. A variety of different treatment options can be used depending on the location of the tumor, size, microscopic characteristics, health of the patient, and other factors. Most therapies are relatively minor office-based procedures that require only local anesthesia. Surgical excision to remove the entire cancer is the most commonly used treatment. "Mohs" micrographic controlled surgery, a method which requires specialized training by dermatologic surgeons, can be used to remove the tumor while sparing as much normal skin as possible. Other dermatologic surgical procedures include laser surgery, cryosurgery (liquid nitrogen - the frozen method), radiation therapy, and electrodesiccation and curettage which involves alternately scraping and cauterizing (burning) the tumor with low levels of electricity.
Spider Veins are very small veins caused by a dilation of the small venules under the skin. This occurs when the pressure inside the vein increases enough to overcome normal resistance of the vein wall. The ability of veins to resist increased pressure is reduced with hormonal changes.
Reticular Veins are small, bluish-colored veins that carry blood to the skin venules and are larger than spider veins. These veins have thin walls and dilate with excessive venous pressure. When this occurs, they become large enough to be unsightly, but are not considered to be varicose veins.
In recent years medical lasers have made great advancements in sophistication. Today, lasers are safely used for a wide variety of cosmetic non-invasive treatments. Laser Therapy treatment is extremely safe and effective on leg veins, as well as veins visible on the face, neck, and chest. Laser treatment also corrects benign pigmented lesions such as age spots and birthmarks. These non-invasive treatments are increasingly popular because they have very few side effects, and one can resume regular activities immediately following treatment.
Both men and women, light and dark-skinned individuals can now safely and effectively benefit from laser therapy for spider veins. Patients using blood thinners or afflicted with a serious illness generally are not candidates for treatment. Patients with dark suntans or photosensitivity disorders, uncontrolled or severe diabetes, bleeding disorders, or those currently taking photosensitizing medications may also be restricted from candidacy.
The number of treatments necessary to resolve your vein concerns depends on the size of the vein and your body's ability to heal. During your consultation, you will be given an estimate of the number of treatments required to obtain optimal results.
Treatment may vary from 15 to 30 minutes. As a result of treatment, the walls of the veins are damaged by the laser's heat. The body next induces a healing process. The veins shrink and become less visible or disappear altogether. Medical studies have documented exceptional results on veins with laser treatments.
The beauty of this treatment is that there is no down time involved. You can resume most of your regular activities immediately. Your doctor may use various methods to reduce the pain that may be associated with this procedure. Swelling and mild bruising can occur, but almost always resolve over a short period of time. Limiting sun exposure, avoiding strenuous exercise, and wearing compression stockings will greatly minimize the risk of complications immediately following your treatment.
Laser Therapy treats many types of leg veins, including shallow spider veins and reticular veins.
Spider Veins are very small veins caused by a dilation of the small venules under the skin. This occurs when the pressure inside the vein increases enough to overcome normal resistance of the vein wall. The ability of veins to resist increased pressure is reduced with hormonal changes.
Reticular Veins are small, bluish-colored veins that carry blood to the skin venules and are larger than spider veins. These veins have thin walls and dilate with excessive venous pressure. When this occurs, they become large enough to be unsightly, but are not considered to be varicose veins.
Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
Just like a precious piece of jewlery or a beautiful piece of furniture, the skin can become dull, weathered and aged. With the modern age of dermatology one can restore the brightness, alleviate lines, get rid of dark marks, erase broken capillaries and scars with no social downtime and superior cosmetic results.
Cosmetic Consultation Reimbursement policy offered to all patients. Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
Skin Cancer is the cancer you can see! Yet skin cancer often goes undetected. With over 5 million cases of skin cancer diagnosed in the U.S. each year, skin cancer is America's most common cancer. More people are diagnosed with skin cancer each year in the U.S. than all other cancers combined.
Types of skin cancers include: Basal Cell Carcinoma, Squamous Cell Carcinoma, Melanoma and Merkel Cell Carcinoma, they are mainly caused by UV exposure to ultraviolet (UV) radiation from the sun. However, skin cancer can form anywhere on the body even if it is not exposed to the sun. All ethnicities and skin tones are at risk.
Basal Cell Carcinoma is the most common skin cancer. It is also one of the easiest to spot and treat. Squamous Cell Carcinoma is the second most common skin cancer and Melanoma the third. Despite Melanoma being the third most common form of skin cancer, it accounts for 75% of all skin cancer deaths.
Basal Cell Carcinomas are quite common, and the number of reported cases in the U.S. is steadily increasing. An estimated 3.6 million cases of Basal Cell Carcinomas are diagnosed each year in the U.S..
Squamous Cell Carcinoma is the second most common. An estimated 1.8 million cases are diagnosed each year in the U.S. which translates to about 205 cases every hour. SCC incidence has increased up to 200% in the past three decades.
Melanoma is the third most common and deadly cancers. Early detection is critical! In the past decade (2012-2022) the number of new invasive melanoma cases diagnosed annually increased by 31%. An estimated 197,700 cases of melanoma will be diagnosed in the U.S. in 2022 and 7,650 people will die of melanoma in 2022. (5,080 men & 2,570 women).
Merkel Cell Carcinoma is about three - five times more likely to be deadly than melanoma. Approximately 3,000 new cases of Merkel Cell Carcinoma are diagnosed annually in the U.S.
The good news is that skin cancer can be prevented, and it can almost always be cured when it’s found and treated early.
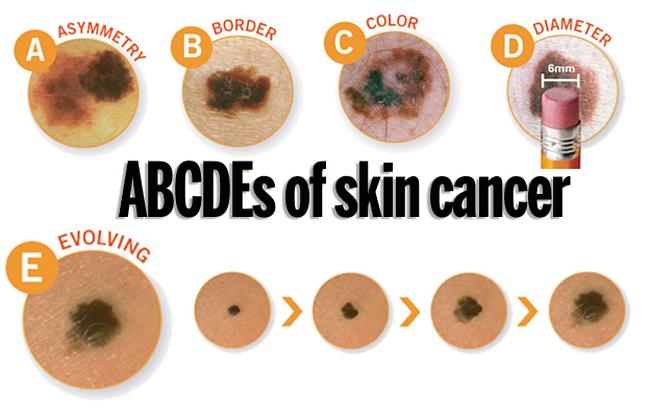
A change in your skin is the most common sign of skin cancer. This could be a new growth, a spot that doesn’t look like others on your body, a sore that doesn’t heal, or a change in a mole. The “ABCDE rule” can be used as a guide. The “ABCDE rule” can be used as a guide (see below).
Skin cancer isn't going to check itself out. Therefore, an annual skin check by a board-certified dermatologist and a monthly skin check by you is vital to good skin care. See something NEW, keep an eye out for any New moles or blemishes that have popped up, CHANGING, a leopard's spots don't change and neither should yours, always check if your spots are Changing in color, size, shape, or texture, or UNUSUAL, one of these things is not like the others ... look for spots that are unusual in outline or continuously itch, hurt, crust or bleed for more than 3 weeks. It could be skin cancer.
When these skin cancers are detected early, treatment often results in a cure. Be sure to schedule an yearly skin exam with your dermatologist and more often if you have a family history of skin cancer.
Take these simple steps today to protect your skin:
Dr. Robinson is improving skin cancer treatments with less invasive treatments. No scarring, no bleeding, functional & cosmetic results are superior to cold steel excision & MOHS. Patients on anticoagulant therapy do not have to stop their medication before treatment, therefore not increasing their risk for stroke and/or heart attack, quick healing, & no risk of post-operative complications! This is especially helpful with Infirm or older patients, great for professionals who can't afford downtime or a scar.
Using non-ablative fractional laser therapy offers a Gentle Approach to Treating Pre-Cancerous Growths and Overall Healthier Skin.
Skin cancer is the most prevalent cancer in the United States. More than 3 million Americans are diagnosed with non-melanoma skin cancer(s), such as basal cell & squamous cell carcinoma each year. These two types of cancers are collectively known as keratinocyte carcinoma or (KC).
In individuals with a history of a prior KC, the risk of developing subsequent KC remains a significant concern.
In our study using non-ablative fractional laser therapy, including 4 sessions spaced at 2-4 week intervals, w/ follow-up assessments, 1-3 months after the final treatment session 60% had greater reduction of the development of KC and had improved overall health of sun-damaged skin. There was also a lower recurrence rate of MOHS. Lowering the rate of infection directly related to lack of having an open wound.
Non-ablative fractional laser therapy has already demonstrated remarkable success with minimal downtime & discomfort as a gentle yet effective treatment of actinic keratosis (AK), the most common type of pre-cancerous skin conditions. Other benefits to using non-ablative fractional laser therapy is it's ability @ ameliorating photo damage, utilizing precise photothermolysis to stimulate collagen and elastin production, promote dermal wound healing & decreasing and improving hyperpigmentation, telangiectasias, skin tone, skin laxity, and tactile roughness. Now we can add treatment of certain skin cancers to the list.
Seborrheic Keratoses are often confused with warts or moles, but they are quite different. Seborrheic Keratoses are non-cancerous growths of the outer layer of skin. There may be just one growth or many which occur in clusters. They are usually brown, but can vary in color from light tan to black and range in size from a fraction of an inch in diameter to larger than a half-dollar. A main feature of Seborrheic Keratoses is their "waxy, pasted-on" appearance. They sometimes look like a dab of warm brown candle wax that has dropped onto the skin or like barnacles attached to the skin.
The exact cause of seborrheic keratoses is unknown; however, they seem to run in families. They are not caused by sunlight and can be found on both sun-exposed and non sun-exposed areas. Seborrheic Keratoses are more common and numerous with advancing age. Although Seborrheic Keratoses may first appear in one spot and seem to spread to another, they are not contagious.
Anyone may develop Seborrheic Keratoses. Some people develop many over time, while others develop only a few. As people age, they may simply develop more. Children rarely develop Seborrheic Keratoses. Seborrheic Keratoses may erupt during pregnancy, following estrogen therapy, or in association with other medical problems.
Seborrheic Keratoses are most often located on the chest or back, although they also can be found on the scalp, face, neck, or almost anywhere on the body. The growths usually begin one at a time as small, rough, itchy bumps which eventually thicken and develop a warty surface.
Seborrheic Keratoses are benign (non-cancerous) and are not serious. Unless they develop suddenly, they do not indicate a serious health problem. They may be unsightly, especially if they appear on the face. Removal may be recommended if they become large, irritated, itch, or bleed easily. A Seborrheic Keratosis may turn black and may be difficult to distinguish from skin cancer. Such a growth must be removed and biopsied (studied under a microscope) to determine if it is cancerous or not.
Creams, ointments, or other medication can neither cure nor prevent Seborrheic Keratoses. Most often Seborrheic Keratoses are removed by cryosurgery, curettage, or electrosurgery. Cryosurgery, liquid nitrogen, a very cold liquid gas, is applied to the growth with a cotton swab or spray gun to "freeze" it. A blister may form under the growth which dries into a scab-like crust. The Keratosis usually falls off within a few weeks. Occasionally, there will be a small dark or light spot that usually fades over time.
Curettage: The keratosis is scraped from the skin. An injection or spray is first used to anesthetize (numb) the area before the growth is removed (curetted). No stitches are necessary, and the minimal bleeding can be controlled by applying pressure or the application of a blood-clotting chemical.
Electrosurgery: The growth is anesthetized (numbed) and an electric current is used to burn the growth which is then scraped off.
Seborrheic dermatitis is a common skin disorder that can be easily treated. This condition is a red, scaly, itchy rash most commonly seen on the scalp, sides of the nose, eyebrows, eyelids, skin behind the ears, and middle of the chest. Other areas, such as the navel (belly button), buttocks, skin folds under the arms, auxillary regions, breasts, and groin, may also be involved.
Your doctor will likely be able to determine whether you have seborrheic dermatitis by examining your skin. He or she may scrape off skin cells for examination (biopsy) to rule out conditions with symptoms similar to seborrheic dermatitis, including:
Dandruff appears as scaling on the scalp without redness. Seborrhea is excessive oiliness of the skin, especially of the scalp and face, without redness or scaling. Patients with Seborrhea may later develop Seborrheic Dermatitis. Seborrheic Dermatitis has both redness and scaling.
This condition is most common in three age groups - infancy, when it's called cradle cap, middle age, and the elderly. Cradle cap usually clears without treatment by age 8 to 12 months. In some infants, Seborrheic Dermatitis may develop only in the diaper area where it could be confused with other forms of diaper rash. When Seborrheic Dermatitis develops at other ages it can come and go. Seborrheic Dermatitis may be seasonally aggravated particularly in northern climates; it is common in people with oily skin or hair, and may be seen with acne or psoriasis. A yeast-like organism may be involved in causing Seborrheic Dermatitis.
Seborrheic Dermatitis may get better on its own, but with regular treatments, the condition improves quickly.
There is no way to prevent or cure Seborrheic Dermatitis. However, it can be controlled with treatment.
Medicated shampoos, creams and lotions are the main treatments for seborrheic dermatitis. Your doctor will likely recommend you try home remedies, such as over-the-counter dandruff shampoos, before considering prescription remedies. If home remedies don't help, talk with your doctor about trying these treatments.
Today, there are many treatment options which, when properly chosen for the specific type of scar and/or skin type, can greatly improve and repair your skin to its natural and more healthy state. These treatment options include surgical excision, laser skin resurfacing, laser skin rejuvenation, intense pulsed light skin rejuvenation, microdermabrasion, chemical peels, dermabrasion, cortisone injections, and bleaching or age defying softening topicals.
During your consultation, your skin type and scar will be evaluated and a customized treatment program will be developed. This may include a combination of treatments to optimize your results. In some cases, certain types of scars can only be improved and not completely eliminated. Your treatment expectations and results will be thoroughly discussed during your consultation.
This option is typically for scars that are deeply pitted, raised, or for older surgical scars that did not heal properly. The scar tissue is removed, followed by careful stitching of the skin to leave a much smaller or thinner scar line.
This treatment is excellent for acne scarring as well as sun damaged or aged skin. The laser vaporizes the damaged skin and commences the regeneration of fresh skin during the following weeks. The thermal damage to the deep tissue stimulates new skin growth, promoting a healthy new collagen layer as well.
Microdermabrasion is a non-surgical exfoliating treatment helpful for those unhappy with scars, acne scars, sun-damaged skin, pigmentation spots, stretch marks, fine lines, and rough skin. Treatment can be performed anywhere on the body. This treatment works for scarring especially when used in conjunction with other modalities.
This is a non-invasive approach in which the laser energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars.
Depending on the skin type and scar to be treated, a superficial, medium, or deep chemical peel may be recommended. In addition to removing the top layers of the epidermis, chemical peels are noted for their ability to stimulate collagen synthesis and aid in the production of new skin cells. Depending on the type of peel, multiple treatments may be required.
This is a non-invasive approach in which intense pulsed light energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars and coarse, uneven skin texture.
By the time we reach our adult years, our skin has been exposed to rough childhood environmental damage, acne, chicken pox, scrapes, burns and numerous other phenomena. As part of the skin’s natural healing process, a scar is formed when several layers of the skin have been damaged. Presently there are diverse treatment modalities available to address various forms of skin scarring. These treatments can dramatically reverse, improve, and renew your skin to it’s natural, healthier state. Many patients seek solutions not only to achieve healthy-looking skin, but also to improve their image and self esteem.
Scabies is an infestation of the skin by the human itch mite. The tiny mites burrow into the upper layer of the skin where it lives and lays its eggs. It has infested humans for at least 2,500 years. It is often hard to detect, and causes a fiercely itchy skin condition. Dermatologists estimate that more than 300 million cases of scabies occur worldwide every year. The condition can strike anyone of any race or age, regardless of personal hygiene. The good news is that with better detection methods and treatments, scabies does not need to cause more than temporary distress.
The microscopic mite that causes scabies can barely be seen by the human eye. Being a tiny, eight-legged creature with a round body, the mite burrows in the skin. Within several weeks, the patient develops an allergic reaction causing severe itching; often intense enough to keep sufferers awake all night.
Human scabies is almost always caught from another person by close contact. It could be a child, a friend, or another family member. Everyone is susceptible. Scabies is not a condition only of low-income families and neglected children, although, it is more often seen in crowded living conditions with poor hygiene.
Attracted to warmth and odor, the female mite burrows into the skin, lays eggs, and produces toxins that cause allergic reactions. Larvae, or newly hatched mites, travel to the skin surface, lying in shallow pockets where they will develop into adult mites. If the mite is scratched off the skin, it can live in bedding for up to 24 hours or more. It may take up to a month before a person will notice the itching, especially in people with good hygiene and who bathe regularly.
The earliest and most common symptom of scabies is intense itching, especially at night. Little red bumps like hives, tiny bites, or pimples appear. In more advanced cases, a rash can spread slowly over a period of weeks or months and the skin may be crusty or scaly.
Scabies skin mite is about 0.4mm, just visible to the human eye
The scabies mite is very small, about the size of the tip of a needle and very difficult to see. It’s white to creamy-white in color. It has eight legs and a round body, which you can see if the mite is magnified. Scabies prefers warmer sites on the skin such as skin folds, where clothing is tight, between the fingers or under the nails, on the elbows or wrists, the buttocks or belt line, around the nipples, and on the penis. Mites also tend to hide in, or on, bracelets and watchbands, or the skin under rings. In children, the infestation may involve the entire body including the palms, soles, and scalp. The child may be tired and irritable because of loss of sleep from itching or scratching all night.
Bacterial infection may occur due to scratching. In many cases, children are treated because of infected skin lesions rather than for the scabies itself. Although treatment of bacterial infections may provide relief, recurrence is almost certain if the scabies infection itself is not treated.
Your healthcare provider must order a cream that contains a medicine called permethrin to treat scabies. The cream is applied to your whole body below your head, including the hands, palms, and soles of the feet.
In children with scabies, the cream may need to be applied to the scalp. Be sure that skin is clean, cool and dry before applying the cream.
Permethrin cream is left on the skin for eight to 14 hours and then washed off. (The cream is most often applied at night and washed off in the morning.)
Ivermectin is another option for treating scabies. This is an antiparasitic pill given in a single dose, followed by a second dose one to two weeks later.
If you’re pregnant or lactating, you shouldn’t use ivermectin. If your child weighs less than 35 pounds (15 kilograms), they shouldn’t use ivermectin.
Your provider might also suggest antihistamines, which can be taken by mouth and as a cream, to relieve itching. Your provider will also treat any type of infection that may be present.
The mites that cause scabies are killed after one treatment. The treatment doesn’t need to be repeated unless the infection doesn’t go away or comes back.
The itching may take two to four weeks to go away, even though the mites have been killed.
Red bumps on the skin should go away within four weeks after treatment.
You can prevent spreading scabies by:
Yes. You can get scabies any time that you come into close contact with an infected person.
No, scabies won’t go away on its own. If you don’t treat it, you’ll probably continue to spread the disease to other people. In addition, the constant itching will probably lead to constant scratching and will cause some type of bacterial infection of the skin.
Scabies is treatable, but they can be hard to get rid of completely. Certain forms of scabies are harder to treat, such as the crusted form. In addition, you might need more than one round of treatment to make sure all of the mites are gone.
If you have a rash and it’s so itchy that you can’t sleep, make sure you contact your healthcare provider. You may have scabies, which is an infectious disease. You and other people close to you should be tested and treated. You’ll want to schedule an appointment with Dr. Robinson if you have any kind of skin rash that doesn’t go away and that causes problems for you. Scabies, like many other types of red itchy rashes, can be treated successfully.



