

Today, there are many treatment options which, when properly chosen for the specific type of scar and/or skin type, can greatly improve and repair your skin to its natural and more healthy state. These treatment options include surgical excision, laser skin resurfacing, laser skin rejuvenation, intense pulsed light skin rejuvenation, microdermabrasion, chemical peels, dermabrasion, cortisone injections, and bleaching or age defying softening topicals.
During your consultation, your skin type and scar will be evaluated and a customized treatment program will be developed. This may include a combination of treatments to optimize your results. In some cases, certain types of scars can only be improved and not completely eliminated. Your treatment expectations and results will be thoroughly discussed during your consultation.
This option is typically for scars that are deeply pitted, raised, or for older surgical scars that did not heal properly. The scar tissue is removed, followed by careful stitching of the skin to leave a much smaller or thinner scar line.
This treatment is excellent for acne scarring as well as sun damaged or aged skin. The laser vaporizes the damaged skin and commences the regeneration of fresh skin during the following weeks. The thermal damage to the deep tissue stimulates new skin growth, promoting a healthy new collagen layer as well.
Microdermabrasion is a non-surgical exfoliating treatment helpful for those unhappy with scars, acne scars, sun-damaged skin, pigmentation spots, stretch marks, fine lines, and rough skin. Treatment can be performed anywhere on the body. This treatment works for scarring especially when used in conjunction with other modalities.
This is a non-invasive approach in which the laser energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars.
Depending on the skin type and scar to be treated, a superficial, medium, or deep chemical peel may be recommended. In addition to removing the top layers of the epidermis, chemical peels are noted for their ability to stimulate collagen synthesis and aid in the production of new skin cells. Depending on the type of peel, multiple treatments may be required.
This is a non-invasive approach in which intense pulsed light energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars and coarse, uneven skin texture.
By the time we reach our adult years, our skin has been exposed to rough childhood environmental damage, acne, chicken pox, scrapes, burns and numerous other phenomena. As part of the skin's natural healing process, a scar is formed when several layers of the skin have been damaged. Presently there are diverse treatment modalities available to address various forms of skin scarring. These treatments can dramatically reverse, improve, and renew your skin to it's natural, healthier state. Many patients seek solutions not only to achieve healthy-looking skin, but also to improve their image and self esteem.
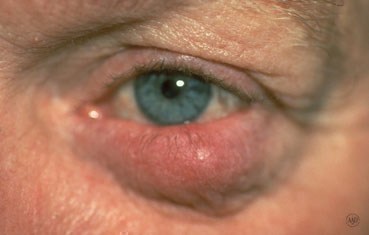
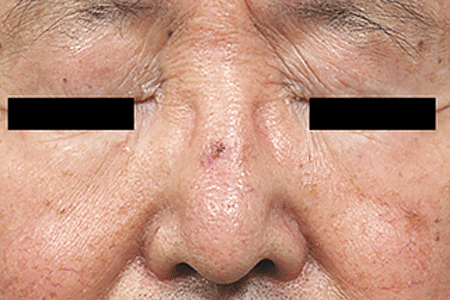
Rosacea is a common skin disease that causes redness, papules, and swelling on the face. Often referred to as adult acne, rosacea frequently begins as a tendency to flush or blush easily. It may progress to persistent redness in the center of the face that may gradually involve the cheeks, forehead, chin, and nose. The eyes, ears, chest, and back may also be involved. With time, small blood vessels and tiny pimples begin to appear on and around the reddened area; however, unlike acne, there are no blackheads.
When rosacea first develops, the redness may come and go. Some people may flush or blush and never form pustules or papules. Small dilated vessels may also be present. However, when the skin doesn't return to its normal color, and when other symptoms such as pimples and enlarged blood vessels become visible, it's best to seek advice from a board-certified dermatologist. The condition may last for years, rarely reverse itself, and can become worse without treatment.
Small red bumps, some of which may contain pus, appear on the face. These may be accompanied by persistent redness and the development of many tiny blood vessels on the surface of the skin.
In more advanced cases, a condition called rhinophyma may develop. The oil glands enlarge causing a bulbous, red nose, and puffy cheeks. Thick bumps may develop on the lower half of the nose and nearby cheeks. Rhinophyma occurs more commonly in men.
Anyone can get Rosacea. It is more common in fair skinned adults between the ages of 30 and 50. Since it may be associated with menopause, women are affected more often than men and may likely have an extreme sensitivity to cosmetics. In people of color, studies show that early symptoms can often be missed and may be under diagnosed because dark skin can mask facial redness. Few children get rosacea, but it is worth considering if the signs and symptoms are there.
Tips for Rosacea Patients
Many people with Rosacea are unfamiliar with it and do not recognize it in its early stages. Identifying the disease is the first step to controlling it. Self-diagnosis and treatment are not recommended since some over-the-counter skin products may make the problem worse.
Dermatologists often recommend a combination of treatments tailored to the individual patient. These treatments can stop the progress of rosacea and sometimes reverse it.
The key to successful management of Rosacea is early diagnosis and treatment. Rosacea can be treated and controlled if medical advice is sought in the early stages. When left untreated, Rosacea will get worse and may be more difficult to treat.





Hemangiomas/Angiomas are growths of blood vessels and other red spots which can be dilated blood vessels that take the form of a birthmark (Nevus Flameus).
Hemangiomas is a bright red birthmark that shows up at birth or in the first or second week of life. It looks like a rubbery bump and is made up of extra blood vessels in the skin. A hemangioma can occur anywhere on the body, but most commonly appears on the face, scalp, chest or back. It can grow out of proportion to the child for the first 8 months of life before the growth rate levels off. Therefore, it is important to evaluate these growths early especially if they are located around the eyes, mouth, genitals, scalp, neck or anus. Many hemangiomas disappear by age 5, and most are gone by age 10. The skin may be slightly discolored or raised after the hemangioma goes away.
Red bumps that we acquire with age or genetics are referred to as cherry angiomas. They often arise later in life and while not dangerous, can be considered unsightly. Their treatment can be simple and often requires no wound care enabling one to return to daily activities immediately.
A doctor can usually diagnose a hemangioma just by looking at it. Tests usually aren't needed.
A hemangioma is made up of extra blood vessels that group together into a dense clump. What causes the vessels to clump isn't known.
Hemangiomas occur more often in babies who are female, white and born prematurely.
Occasionally, a hemangioma can break down and develop a sore. This can lead to pain, bleeding, scarring or infection. Depending on where the hemangioma is situated, it may interfere with your child's vision, breathing, hearing or elimination, but this is rare.
Treating hemangiomas usually isn't necessary because they go away on their own with time. But if a hemangioma affects vision or causes other problems, treatments include medications or laser surgery:
If you're considering treatment for your child's hemangioma, weigh the pros and cons with your child's doctor. Consider that most infantile hemangiomas disappear on their own during childhood and that treatments have potential side effects.
Genital warts affect the moist tissues of the genital area. They can look like small, flesh-colored and be flat or bumpy or have a cauliflower-like appearance. Some genital warts are so small they cannot be seen. They can cause pain, discomfort or itching. Genital warts, also known as venereal warts, or condylomata acuminata, are caused by the human papilloma virus (HPV). More than 100 types of HPV are known to exist. Low risk types (HPV 1, 2, and 3) cause warts on the hands, feet, and other parts of the body. The low risk strains - Types (6 and 11) can cause warts on the genitals or anus (genital warts), and other high risk strains - Types (HPV 16 and 18) can cause cancer of the cervix, external genitalia, vulva, and anus.
Genital warts are sexually transmitted disease (STD) and all partners should be checked thoroughly. They can also be seen in infants who have been delivered vaginally to mothers with HPV in their genital tracts; therefore, alternate methods of delivery should be considered.
Only a small percentage of people infected with HPV will develop genital warts. Many people are carriers of HPV who may never develop warts, but may still be able to pass HPV to their sexual partners. The incubation period from contracting HPV until the development of warts may be several months although some people may not develop warts for years after contact with HPV. People who have lower immunity due to cancer, AIDS, organ transplantation, immune suppressive medications, or certain other medications are more susceptible.
To diagnose this condition, your doctor will do the following:
Although HPV isn't curable in all cases, genital warts are treatable. You can also go extended periods of time without an outbreak, but it may not be possible to get rid of the warts forever. That's because genital warts are only a symptom of HPV, which may become a chronic, lifelong infection for some.
If you've developed genital warts, your doctor has a few options for treatment. The fastest way to remove them is through surgery or to freeze them off with liquid nitrogen. Some doctors might use an electric current or laser treatment to burn off the warts.
Genital warts can go away with treatment from your healthcare provider or with prescription medicine. If left untreated, genital warts may go away, stay the same, or grow in size or number. Cervical precancer treatment is available.
Your doctor may apply a mild acidic solution, called an acetowhite test, to your skin to help make genital warts more visible. It may cause a slight burning sensation.
If you have a vulva, your doctor may also need to perform a pelvic examination, because genital warts can occur deep inside your body.
While visible genital warts often go away with time, HPV itself can linger in your skin cells. This means you may have several outbreaks over the course of your life.
So managing symptoms is important because you want to avoid transmitting the virus to others. That said, genital warts can be passed on to others even when there are no visible warts or other symptoms.
You may wish to treat genital warts to relieve painful symptoms or to minimize their appearance. However, you can’t treat genital warts with over-the-counter (OTC) wart removers or treatments.
Your doctor may prescribe topical wart treatments that might include:
If visible warts don’t go away with time, you may need minor surgery to remove them. Your doctor can also remove warts through these procedures:
To help prevent genital warts, HPV vaccines, condoms, and other barrier methods are available:
If you think you have genital warts, talk with your doctor. They can determine if you have warts and what your best treatment options are.
In addition, it’s important to talk with your sexual partner. This may sound difficult, but being open about your condition can help you protect your partner from also getting an HPV infection and genital warts.
Genital warts are a complication of a low risk HPV infection that’s common and treatable. They can disappear over time, but treatment is essential in preventing their return and possible complications.
Laser treatment can be utilized for small facial areas or for the entire face. Recently, full face treatments have become increasingly popular. Many people suffer from larger broken capillaries on their nose and cheeks and will have medium and smaller vessels on other facial areas. A full-face treatment will improve the overall facial appearance by creating a more uniform skin color, and by smoothing the texture of the skin.
Light emitted from the handpiece safely passes through the outermost layers of skin in search of the targeted vascular or pigmented lesions. Without damaging the surrounding skin, the lasers intense light is absorbed by the targeted lesion. The light energy is then converted to heat and this initiates the process of eliminating the lesion. The treated lesion will gradually fade or diminish. In many cases, smaller vessels or pigmentation spots are eliminated in 2 to 4 treatments. Medium or larger vessels may take additional treatments.
The hand piece quickly advances across the skin delivering pulses to the treatment site. A full-face treatment typically lasts anywhere from 20 to 40 minutes. Smaller areas, such as the nose, can be treated in 15 minutes. In some cases a topical anesthetic cream is first applied to numb the treatment area. For a short period of time following treatment, a cold compress may be applied to soothe the possible appearance of slight swelling or redness of the skin. Treatments on the face, chest, neck, hands, legs, and abdomen are all done safely and quickly with laser technology.
During your consultation, your skin's condition will be evaluated and a customized treatment program will be suggested. In some cases only one or two treatments are required. However, in many cases three to five or more treatments will be required to achieve premium results. The number of treatment sessions will depend on the type of lesion to be treated, the location of the lesion on the body, and its size and color. In many cases, it is recommended that treatments applied to the face be repeated at 3 to 4 week intervals. The time intervals of your treatments will be determined during the consultation, where many of these issues and concerns may be addressed.
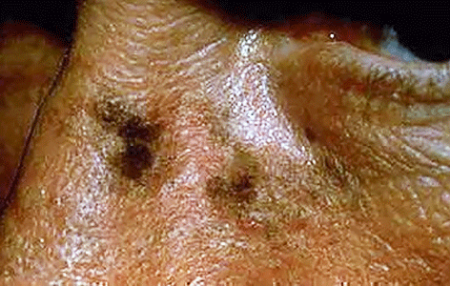
Age spots are small, flat dark areas on the skin. They vary in size and usually appear on areas exposed to the sun, such as the face, hands, shoulders and arms. Age spots are also called sunspots, liver spots and solar lentigines.
Age spots can look like cancerous growths. True age spots don't need treatment, but they are a sign the skin has received a lot of sun exposure and are an attempt by your skin to protect itself from more sun damage. You can help prevent age spots by regularly using sunscreen and avoiding the sun.
Age spots may affect people of all skin types, but they're more common in adults with light skin. Unlike freckles, which are common in children and fade with no sun exposure, age spots don't fade.
Age spots don't require medical care. Have your doctor look at spots that are black or have changed in appearance. These changes can be signs of melanoma, a serious form of skin cancer.
It's best to have any new skin changes evaluated by a doctor, especially if a spot:
Age spots are caused by overactive pigment cells. Ultraviolet (UV) light speeds up the production of melanin, a natural pigment that gives skin its color. On skin that has had years of sun exposure, age spots appear when melanin becomes clumped or is produced in high concentrations. Also, the use of commercial tanning lamps and beds can cause age spots.
We offer a range of advanced laser therapies tailored to the type and depth of discoloration, whether you’re dealing with brown spots, melasma, sun damage, or red marks from acne or rosacea. Each treatment is selected based on your unique skin tone, condition, and goals.
Lasers for Brown Spots, Melasma & Sun Damage:
These lasers use ultra-short pulses to break up unwanted pigment while minimizing damage to surrounding skin, ideal for darker skin tones.
Q-switched Nd:YAG Laser: Targets deep pigmentation, including melasma and post-inflammatory hyperpigmentation (PIH), with precision and safety for all skin tones.
Fractional Lasers: These versatile lasers treat pigmentation and improve overall skin quality by stimulating collagen production and resurfacing the skin. Great for: PIH (post inflammatory hyperpigmentation), sun damage, acne scarring, uneven tone, and texture.
Vascular Lasers:
Specialized for redness and pink-toned PIH (post inflammatory hyperpigmentation), especially from acne or rosacea.
Vbeam (Pulsed Dye Laser):
Targets blood vessels to reduce red marks, flushing, and inflammation. A gentle, effective option for sensitive or reactive skin types.
Each laser treatment is customized to your skin’s needs to ensure safe, effective results. During your consultation, we’ll determine the best approach—often combining laser therapy with topical treatments to maximize improvement and minimize recurrence.
For brown marks on deeper skin tones, we use a combination of hydroquinone, kojic acid, Vitamin C, and AHAs to gently and effectively lighten dark spots while brightening and smoothing the skin.
These clinically proven ingredients work synergistically to visibly brighten, lighten, and tighten the skin, revealing a more even, radiant complexion.
JAS Anti - Aging TRIO, expertly formulated to replenish, exfoliate, and restore your skin’s natural glow.
To help avoid age spots and new spots after treatment, follow these tips for limiting your sun exposure:
⚠️ Important
Always see a board-certified dermatologist or laser specialist, especially if you have darker skin.
Sun protection is non-negotiable—exposure after treatment can trigger new pigment.
If you are tired of looking older or want the spots removed, schedule a laser consultation and restore your skin to its natural beauty. Our Cosmetic Consultation Reimbursement policy is offered to all patients. Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
Birthmarks are abnormalities of the skin that are present when a baby is born.
A birthmark can be red or brown.
A red or vascular birthmark is made up of dilated blood vessels. Two types are hemangiomas and port-wine stains. Although they can resolve spontaneously on their own, some can cause deformities and become more purple in color. With the advent of laser treatment, the Nevus Flameus can be cleared and subsequent deformities prevented.
A Nevus of Ota, Nevus of Ito and Mongolian spot are brown to bluish birthmarks that usually occur around the eye, shoulder and trunk respectively. Given their size and location patients often consider them cosmetically unacceptable, using the Medlite Nd:Yag laser these birthmarks can be treated effectively with excellent results.
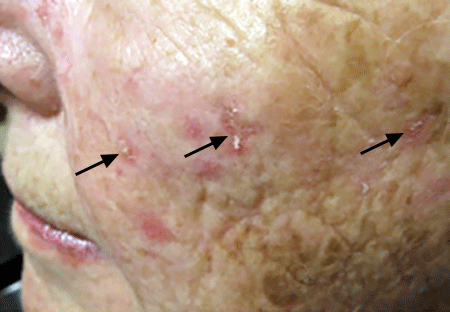
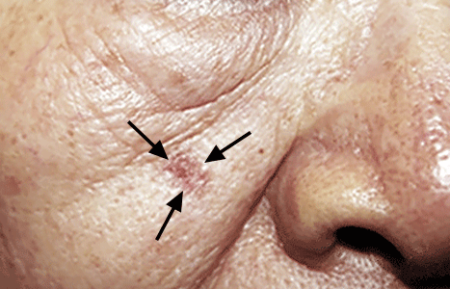
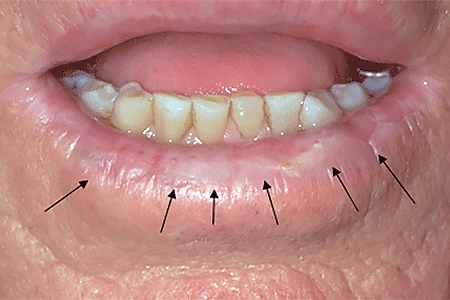
An actinic keratosis, is a rough, scaly patch on the skin that develops from years of sun exposure. It's often found on the face, lips, ears, forearms, scalp, neck or back of the hands. These represent pre-cancerous growths that can become skin cancer if left untreated.
If you find a spot or growth on your skin that you think could be an actinic keratosis (AK), it’s time for a thorough skin exam. Should you have an AK, an accurate diagnosis and treatment can:
Most people who have AKs (or think they may have an AK) see a dermatologist. This is actually one of the most common conditions that dermatologists diagnose and treat.
When you see a board-certified dermatologist about AKs, your dermatologist will:
If you have one or more AKs on your skin, a board-certified dermatologist can often diagnose you by looking carefully at your skin. While examining your skin, your dermatologist will also look for signs of skin cancer. People who have skin that’s been badly damaged by ultraviolet (UV) light develop AKs and have a higher risk of getting skin cancer.
If you have one or more AKs, your dermatologist will talk with you about whether to treat these precancerous skin growths. Usually, treatment is recommended.
For a few people, a dermatologist may recommend frequent skin exams rather than treatment. Skin exams are recommended for patients who are frail and may find it hard to tolerate treatment. To be effective, treatment must destroy the AKs. When this happens, your skin will feel raw. It may be red and swollen for a brief time.
The treatment that is right for you depends on several considerations, including:
If you have one or a few AKs, a procedure that your dermatologist can perform during an appointment may be the preferred treatment.
You can often complete treatment in 1 or 2 office visits. The procedures that dermatologists use to treat AKs include:
Some people develop a few AKs, which can often be cleared with treatment.
If you have many AKs, it’s a good idea to be under a dermatologist’s care. Your skin has been severely damaged by UV light, so it’s likely you’ll continue get new AKs. You may also develop skin cancer. Your dermatologist can watch for signs of new AKs and skin cancer. When found early and treated, skin cancer is highly treatable.
Your dermatologist will tell you how often to return for check-ups. Some people need a check-up once or twice a year. If you have a weakened immune system or a rare condition that greatly increases your risk of developing AKs and skin cancer, you may need to see your dermatologist every 8 to 12 weeks.
Keep every appointment. If skin cancer develops, the sooner it is found and treated, the better your outcome.
Self-care also plays a key role in your outcome. The right self-care can help to prevent new AKs and skin cancer.


Acne is a skin condition which has plugged pores (blackheads and whiteheads), inflamed pimples (pustules), and deeper lumps (nodules). Acne occurs on the face, as well as the neck, chest, back, shoulders, and upper arms. Although most teenagers get some form of acne, adults in their 20's, 30's, 40's, or even older, can develop acne. Often, acne clears up after several years, even without treatment. Acne can be disfiguring and upsetting to the patient. Untreated acne can leave permanent scars; these may be treated by your dermatologist in the future. To avoid acne scarring, treating acne is important.
Acne is not caused by dirt. Testosterone, a hormone which is present in both males and females, increases during adolescence (puberty). It stimulates the sebaceous glands of the skin to enlarge, produce oil, and plug the pores. Whiteheads (closed comedones), blackheads (open comedones), and pimples (pustules) are present in teenage acne.
Early acne occurs before the first period and is called prepubertal acne. When acne is severe and forms deep "pus-filled" lumps, it is called cystic acne. This may be more common in males. Adult acne develops later in life and may be related to hormones, childbirth, menopause, or stopping the pill. Adult women may be treated at the period and at ovulation when acne is especially severe, or throughout the entire cycle. Adult acne is not rosacea, a disease in which blackheads and whiteheads do not occur.
Acne has nothing to do with not washing your face. However, it is best to wash your face with a mild cleanser and warm water daily. Washing too often or too vigorously may actually make your acne worse.
Acne is not caused by foods. However, if certain foods seem to make your acne worse, try to avoid them.
Wear as little cosmetics as possible. Oil-free, water-based moisturizers and make-up should be used. Choose products that are "non-comedogenic" (should not cause whiteheads or blackheads) or "non-acnegenic" (should not cause acne). Remove your cosmetics every night with mild soap or gentle cleanser and water.
A flesh-tinted acne lotion containing acne medications can safely hide blemishes. Loose powder in combination with an oil-free foundation is also good for cover-up.
Shield your face when applying sprays and gels on your hair.
Control of acne is an ongoing process. All acne treatments work by preventing new acne breakouts. Existing blemishes must heal on their own, and therefore, improvement takes time. If your acne has not improved within two to three months, your treatment may need to be changed. The treatment your dermatologist recommends will vary according to the type of acne.
Occasionally, an acne-like rash can be due to another cause such as make-up or lotions, or from oral medication. It is important to help your dermatologist by providing an updated history of what you are using on your skin or taking internally.
Many non-prescription acne lotions and creams help mild cases of acne. However, many will also make your skin dry. Follow instructions carefully.
Re-think your skin health. Hydrafacial MD, - * Acne Facial, is highly effective for anyone suffering from oily and/or acne-prone skin. It visibly reduces redness, enlarged pores, hyperpigmentation, utilizing LED blue light killing acne causing bacteria. HydraFacial MD - Hydradermabrasion is the latest, non-invasive, "gentle" skin resurfacing and complexion treatment. The immediate, noticeable, long lasting results are achieved with zero downtime and without any discomfort. You can return to school, work, social life, or exercise right after your procedure. HydraFacial MD uses a uniquely shaped spiral tip and patented vortex fusing technology to gently cleanse, exfoliate, and extract, removing impurities and dead skin cells while hydrating the skin and adding antioxidant protection simultaneously.
Acne scars no longer have to be lived with forever. Often occurring on the face, back and chest these scars can now be treated with a variety of lasers (Fraxel®, V-Beam), subcission or chemical peels. These treatments require no social downtime and can be performed on all skin colors.
Vbeam® Perfecta laser is the gold standard to target sun damage, rosacea, and a variety of red broken and damaged blood vessels & other vascular skin conditions, with no downtime. V-Beam helps with Rosacea, stretch marks, Keloid scars, leg veins, spider veins, dilated blood vessels and other conditions.
Additionally, Dr. Robinson can utilize the Vbeam® Perfecta laser to target melanin in pigmented lesions, such as age spots, freckles, and sunspots. The energy from the laser breaks down the excess melanin, allowing the body’s natural healing processes to fade the pigmented lesions over time gradually. It helps rejuvenate healthy skin naturally and restore a softer, smoother skin texture and tone.
The treatment is precise and controlled, minimizing damage to surrounding tissues and reducing the risk of side effects. It also stimulates collagen production, promoting skin rejuvenation and improving overall skin texture and tone.
Vbeam Perfecta is suitable for various skin types and can be used on the face, neck, chest, hands, and other body areas. The procedure is quick, typically lasting between 15 to 30 minutes, and requires minimal downtime, allowing patients to resume their daily activities immediately after treatment.
A Vbeam® laser is a minimally invasive, pulse-dye laser that safely delivers short bursts of light to the treatment area. The light beam targets and coagulates broken and damaged blood vessels and vascular lesions so they may be naturally reabsorbed by your body during the healing process.
After a comprehensive assessment including a skin examination and medical history, Dr. Robinson will design a treatment plan for you. You will be provided with protective eyewear to shield your eyes during the treatment. Using a small hand piece, Dr. Robinson will deliver short bursts of light, lengthening in duration, with puffs of cryogen cooling mist. The treatment is safe and comfortable. Many patients notice improvement after a single treatment, but 3-5 sessions are typically recommended for optimal results. These results can last up to 18 months. Dr. Robinson will recommend a schedule that is right for you.
You should avoid saunas, hot tubs, and other forms of excessive heat for 48 hours after treatment. For the first two weeks avoid skincare products that may clog your pores or cause skin irritation. As with all skin treatments, it is critical to use a SPF 30 or higher sunscreen every time you go outdoors.
Whether used to address specific skin concerns or as part of a comprehensive skincare regimen, Vbeam® Perfecta offers a versatile solution for achieving radiant, youthful-looking skin.
If you’re considering Vbeam® Perfecta laser skin treatment, take the first step towards healthier, more radiant skin by consulting with Dr. Robinson to assess your skin concerns, discuss your treatment goals, and determine if Vbeam® Perfecta is the right option. With our expertise and guidance, you can ensure that you receive personalized care and achieve the best possible results.
Our Cosmetic Consultation Reimbursement policy is offered to all our patients. Come discuss your needs and goals with Dr. Robinson and the office visit cost will be applied to future costs for the discussed procedure. Procedure must be completed within 30 days of your consult visit.

