

Shingles causes a painful, blistering rash on your skin. If you get shingles, you may notice the following three stages:
Before the rash appears: For 1 to 2 days before the rash appears, you may have pain, burning, or tingling on an area of skin where the rash will develop. Some people have described an “electrical sensation” on their skin before getting the rash.
Rash appears: A painful, blistering rash appears. It usually appears on one side of your body, often on the torso; however, it can appear anywhere on your skin. Some people get more blisters after the rash appears, so it can seem that the rash is spreading.
Rash starts to clear: As the rash clears, the blisters may crack open, bleed, and scab over. For most people, the rash will clear within 2 to 4 weeks.
If you have a rash of blisters on your skin or a rash that looks like those shown below, schedule an appointment immediately for a diagnosis. If you have shingles, it’s important to get treatment, preferably within 1 to 3 days.
If you’ve had the rash for longer than 2 to 3 days, it’s still important to schedule an appointment!
Along with a painful, blistering rash, some people can also have one or more of the following:
Rash: PLEASE call our office to schedule an appointment immediately or other health-care provider within 3 days of getting the rash. When treatment is started within 3 days, treatment can prevent possible complications, such as long-lasting nerve pain.
Receiving treatment after 3 days still has benefits, so you should still schedule an appoointment to see your doctor if you’ve had the rash for longer than 3 days.
Before taking any medication, it’s important to make sure that you have shingles.We will prescribe an antiviral medication. One of three antiviral medications is usually prescribed—acyclovir, famciclovir, or valacyclovi to:
Pain: Over-the-counter medication(s) can help, such as:
If you have severe pain, we may prescribe a medication that reduces inflammation, such as a corticosteroid.
Talk with your doctor about getting the shingles vaccine, Shingrix. You can get shingles again. A shingles vaccine that the U.S. Food and Drug Administration (FDA) approved in 2017 can greatly reduce your risk of developing shingles again. You can learn more about this vaccine at, Shingles Vaccine, CDC.
The CDC recommends that adults 50 years and older get two doses of the shingles vaccine called Shingrix (recombinant zoster vaccine) to prevent shingles and the complications from the disease. Adults 19 years and older who have weakened immune systems because of disease or therapy should also get two doses of Shingrix, as they have a higher risk of getting shingles and related complications.
Until the shingles rash clears, you are contagious.
Anyone who has not had chickenpox (or the vaccine for chickenpox) can catch the virus. This could cause chickenpox. To avoid infecting others, who could get chickenpox and later shingles, dermatologists recommend that you do the following until the rash clears:



Having a shingles rash on your face is a medical emergency.
Even if the rash isn’t on your eye, it could still affect your eyesight. Immediately seeing a doctor for treatment could save your eyesight.


The use of repellents can protect both your health and sanity.
While some bug bites leave bothersome, itchy bumps on your skin they can also pose a serious threat and sometimes deadly risk to your health. Insect-borne diseases, may transmit harmful pathogens that can cause dangerous diseases like Lyme disease, Malaria, Dengue fever, Zika, and West Nile.
We have options when it comes to choosing what type of repellent to use -- sprays and lotions, candles, coils and vaporizers to name a few.
These repellents interfere with a mosquito's sense of smell, taste or both. The repellent either blocks or over stimulates these senses.
Bracelets, wristbands and watches. Even if they are loaded with repellents, they can't protect your whole body from getting bitten.
Ultrasonic repellent devices don't work. These come as electrical plug-ins, free standing varieties or watch-like accessories that claim to emit a high frequency sound that deters bugs by mimicking bats.
Dietary Supplements -- vitamin B, garlic, and so on -- don't work.
Light based repellents don't work. These devices come as colored light bulbs and they don't attract insects that fly toward white light. This works well on months, beetles, and stinkbugs but not on mosquitos.
DEET works! DEET, was developed in the 1950's by the US Army and is a well established bug repellent. The higher the percentage, the longer the protection time is -- up to six hours. Despite its sixty year history of use by consumers, how exactly DEET works to keep bugs at bay still isn't fully understood. It's likely that more than one mechanism is at play.
How safe is DEET? Since it was originally used in 1957 a broad scientific consensus still holds that the chemical is safe when used as directed on the label. Newer insect repellent active ingredients are however judged. These need more time to look at outcomes.
Picaridin works. This synthetic repellent can protect for up to six hours at a 20% concentration. This is a promising alternate to DEET.
Oil of lemon eucalyptus, or OLE, works. OLE, with the active ingredient PMD, is a plant-based alternative to DEET and Picaridin. It's repellent properties can last for up to six hours.
Citronella works, just not that great and for not that long.
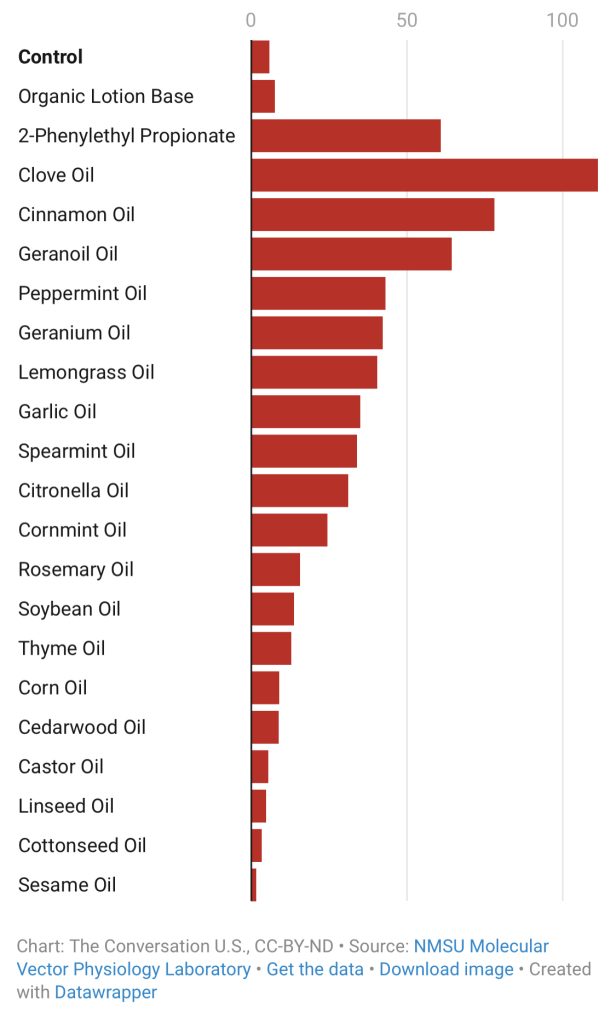
An arm-in-cage experiment for different essential oils has been completed specifically for mosquitos. Complete protection times (in minutes) measured for lotions with a 10% concentration of each essential oil. The longer the complete protection time the better the repellent will protect against mosquitos.
If your planning to mix your own plant-based mosquito repellent, remember that essential oils are complex mixtures of plant-made chemicals that can cause skin irritation.
Based on studies and efficacy we recommend using repellents with the active ingredient DEET that contains at least 20-30 percent DEET on exposed skin and clothing and re-apply as directed. If you are wearing sunscreen and DEET apply sunscreen first.
Sometimes, despite one’s greatest efforts, bug bites still happen. Fortunately, most bug bites and stings can be safely treated at home.
For painful bites, such as a bee sting, take an over-the-counter painkiller, such as acetaminophen or ibuprofen. For bites that itch, apply an ice pack or an over-the-counter anti-itch cream, such as hydrocortisone. Another option is to take an over-the-counter oral antihistamine. Always follow the directions on the label and use the correct dose. If these over the counter remedies do not work schedule an appointment to discuss treatment options that may yield better relief.
If you experience any serious symptoms after a bug bite, such as a rash, fever, or body aches, schedule an appointment immediately. Make sure you tell us about your recent bite so that we can examine you for a transmitted disease.

It is important to treat a sunburn as soon as you notice it.
The first thing you should do if you feel you have or are getting a sunburn is get out of the sun, preferably go indoors. Once indoors, these tips can help relieve the discomfort:
If you have fever, chills, headache or any questions about your sunburn please call our office to schedule an appointment. Although it may seem like a temporary condition, sunburn is a result of skin receiving too much exposure from the sun’s ultraviolet (UV) rays and can cause long-lasting damage to the skin. This damage increases a person’s risk for getting skin cancer.
Skin Cancer is the cancer you can see! Yet skin cancer often goes undetected. With over 5 million cases of skin cancer diagnosed in the U.S. each year, skin cancer is America's most common cancer. More people are diagnosed with skin cancer each year in the U.S. than all other cancers combined.
Types of skin cancers include: Basal Cell Carcinoma, Squamous Cell Carcinoma, Melanoma and Merkel Cell Carcinoma, they are mainly caused by UV exposure to ultraviolet (UV) radiation from the sun. However, skin cancer can form anywhere on the body even if it is not exposed to the sun. All ethnicities and skin tones are at risk.
Dr. Bruce P. Robinson has pioneered a transformative new treatment option for the most common forms of skin cancer: Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC). His new and significant research in the treatment of Basal & Squamous cell carcinoma’s can be seen in the Archives of Dermatological Research, Utilizing fractional lasers and tirbanibulin ointment to treat squamous and basal cell carcinomas with a 99% cure rate to date and no recurrence
Basal Cell Carcinoma is the most common skin cancer and the number of reported cases in the U.S. is steadily increasing. It is also one of the easiest to spot and treat. Squamous Cell Carcinoma is the second most common skin cancer and Melanoma the third. Despite Melanoma being the third most common form of skin cancer, it accounts for 75% of all skin cancer deaths.
Squamous Cell Carcinoma is the second most common. An estimated 1.8 million cases are diagnosed each year in the U.S. which translates to about 205 cases every hour. SCC incidence has increased up to 200% in the past three decades.
Melanoma is the third most common and deadly cancers. Early detection is critical! In the past decade (2012-2022) the number of new invasive melanoma cases diagnosed annually increased by 31%. An estimated 197,700 cases of melanoma will be diagnosed in the U.S. in 2022 and 7,650 people will die of melanoma in 2022. (5,080 men & 2,570 women).
Merkel Cell Carcinoma is about three - five times more likely to be deadly than melanoma. Approximately 3,000 new cases of Merkel Cell Carcinoma are diagnosed annually in the U.S.
The good news is that skin cancer can be prevented, and it can almost always be cured when it’s found and treated early.
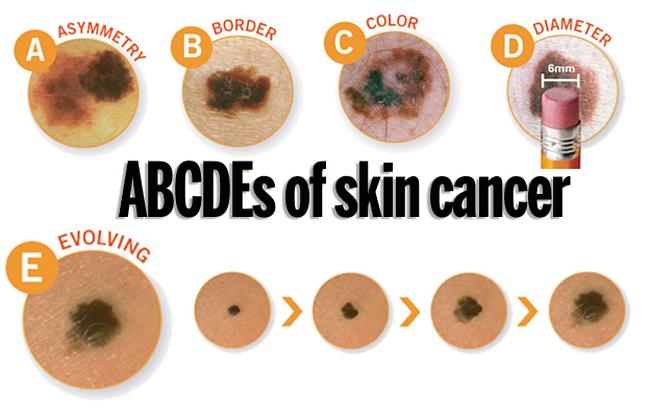
A change in your skin is the most common sign of skin cancer. This could be a new growth, a spot that doesn’t look like others on your body, a sore that doesn’t heal, or a change in a mole. The “ABCDE rule” can be used as a guide. The “ABCDE rule” can be used as a guide (see below).
Skin cancer isn't going to check itself out. Therefore, an annual skin check by a board-certified dermatologist and a monthly skin check by you is vital to good skin care. See something NEW, keep an eye out for any New moles or blemishes that have popped up, CHANGING, a leopard's spots don't change and neither should yours, always check if your spots are Changing in color, size, shape, or texture, or UNUSUAL, one of these things is not like the others ... look for spots that are unusual in outline or continuously itch, hurt, crust or bleed for more than 3 weeks. It could be skin cancer.
When these skin cancers are detected early, treatment often results in a cure. Be sure to schedule an yearly skin exam with your dermatologist and more often if you have a family history of skin cancer.
Take these simple steps today to protect your skin:
Dr. Bruce Robinson is advancing skin cancer treatment with innovative non-invasive techniques that provide superior outcomes compared to traditional methods like surgical excision and Mohs surgery. His approach uses fractional laser technology, which eliminates the need for downtime, scarring, or bleeding, while offering functional and cosmetic results that are more favorable than conventional treatments. This method enhances both patient care and quality of life by reducing the invasiveness of treatment and improving recovery. See Publication Here ...
Skin cancer is the most prevalent cancer in the United States. More than 3 million Americans are diagnosed with non-melanoma skin cancer(s), such as basal cell & squamous cell carcinoma each year. These two types of cancers are collectively known as keratinocyte carcinoma or (KC).
In individuals with a history of a prior KC, the risk of developing subsequent KC remains a significant concern.
Non-ablative fractional laser therapy has already demonstrated remarkable success with minimal downtime & discomfort as a gentle yet effective treatment of actinic keratosis (AK), the most common type of pre-cancerous skin conditions. Other benefits to using non-ablative fractional laser therapy is it's ability @ ameliorating photo damage, utilizing precise photothermolysis to stimulate collagen and elastin production, promote dermal wound healing & decreasing and improving hyperpigmentation, telangiectasias, skin tone, skin laxity, and tactile roughness. Now we can add treatment of certain skin cancers to the list.
Poison ivy, poison oak, and poison sumac are the most common cause of allergic reactions in the United States. Each year 10 to 50 million Americans develop an allergic rash after contact with these poison plants.
Poison ivy, poison oak, and poison sumac grow almost everywhere in the United States, except Hawaii, Alaska, and some desert areas in the Western U.S. poison ivy usually grows east of the Rocky Mountains and in Canada. Poison oak grows in the Western United States, Canada, Mexico (western poison oak), and in the Southeastern states (eastern poison oak). poison sumac grows in the Eastern states and southern Canada.
In the West, this plant may grow as a vine but usually is a shrub. In the East, it grows as a shrub. It has three leaflets to form its leaves in the shape of an oak tree leaf.
Grows as a vine in the East, Midwest and South. In the far Northern and Western United States, Canada and around the Great Lakes, it grows as a shrub. Each leaf has three leaflets.
Grows in standing water in peat bogs in the Northeast and Midwest and in swampy areas in parts of the Southeast. Each leaf has seven to 13 leaflets.
Poison Plant rash is an allergic contact dermatitis caused by contact with oil called urushiol. Urushiol is found in the sap of poison plants like Poison Ivy, Poison Oak, and Poison Sumac. It is colorless or pale yellow oil that oozes from any cut or crushed part of the plant, including the roots, stems, and leaves. After exposure to air, urushiol turns brownish-black. Damaged leaves look like they have spots of black enamel paint making it easier to recognize and identify the plant. Contact with urushiol can occur in three ways:
When urushiol gets on the skin, it begins to penetrate in minutes. A reaction appears usually within 12 to 48 hours. There is severe itching, redness, and swelling, followed by blisters. The rash is often arranged in streaks or lines where the person brushed against the plant. In a few days, the blisters become crusted and take 10 days or longer to heal.
Poison plant dermatitis can affect almost any part of the body. The rash does not spread by touching it, although it may seem to when it breaks out in new areas. This may happen because urushiol absorbs more slowly into skin that is thicker such as on the forearms, legs, and trunk.
Sensitivity develops after the first direct skin contact with urushiol oil. An allergic reaction seldom occurs on the first exposure. A second encounter can produce a reaction which may be severe. About 85 percent of all people will develop an allergic reaction when adequately exposed to poison ivy. This sensitivity varies from person to person. People who reach adulthood without becoming sensitive have only a 50 percent chance of developing an allergy to poison ivy. However, only about 15 percent of people seem to be resistant.
Identifying the poison ivy plant is the first step in avoiding the rash. The popular saying of leaves of three, let it be; is a good rule of thumb for Poison Ivy and Poison Oak, but is only partly correct. A more exact saying would be leaflets of three, beware of me; because each leaf has three leaflets. Poison sumac, however, has a row of paired leaves. The middle or end leaf is on a longer stalk than the other leaves. This differs from most other three-leaf look alikes.
Poison Ivy has different forms. It grows as vines or low shrubs. Poison Oak, with its oak-like leaves, is a low shrub in the East and can be a low or high shrub in the West. Poison sumac is a tall shrub or small tree. The plants also differ in where they grow. Poison Ivy grows in fertile, well-drained soil. Western Poison Oak needs a great deal of water, and Eastern Poison Oak prefers sandy soil but sometimes grows near lakes. Poison Sumac tends to grow in standing water, such as peat bogs.
These plants are common in the spring and summer. When they grow, there is plenty of sap and the plants bruise easily. The leaves may have black marks where they have been injured. Although Poison Ivy rash is usually a summer complaint, cases may occur in winter when people are cleaning their yards and burning wood with urushiol on it, or when cutting Poison Ivy vines to make wreaths.
It is important to recognize these toxic plants in all seasons. In the early fall, the leaves can turn colors such as yellow or red when other plants are still green. The berry-like fruit on the mature female plants also changes color in fall, from green to off-white. In the winter, the plants lose their leaves. In the spring, Poison Ivy has yellow-green flowers.
Prevent the misery of Poison Ivy by looking out for the plant and staying away from it. You can destroy these plants with herbicides in your own backyard, but this is not practical elsewhere. If you are going to be where you know poison ivy likely grows, wear long pants, long sleeves, boots, and gloves. Remember that the plant's nearly invisible oil, urushiol, sticks to almost all surfaces, and does not dry. Do not let pets run through wooded areas since they may carry home urushiol on their fur. Because urushiol can travel in the wind if it burns in a fire, do not burn plants that look like Poison Ivy.
Barrier skin creams such as a lotion containing bentoquatum offer some protection before contact with Poison Ivy, Poison Oak, or Poison Sumac. Over-the-counter products prevent urushiol from penetrating the skin. Ask your dermatologist for details.
If you think you've had a brush with Poison Ivy, Poison Oak, or Poison Sumac, follow these simple ste
Scratching Poison Ivy blisters will spread the rash.
False. The fluid in the blisters will not spread the rash. The rash is spread only by urushiol. For instance, if you have urushiol on your hands, scratching your nose or wiping your forehead will cause a rash in those areas even though leaves did not contact the face. Avoid excessive scratching of your blisters. Your fingernails may carry bacteria that could cause an infection.
Poison Ivy rash;
False. The rash is a reaction to urushiol. The rash cannot pass from person to person; only urushiol can be spread by contact.
Once allergic, always allergic to Poison Ivy.
False. A person's sensitivity changes over time, even from season to season. People who were sensitive to Poison Ivy as children may not be allergic as adults.
Dead Poison Ivy plants are no longer toxic.
False. Urushiol remains active for up to several years. Never handle dead plants that look like Poison Ivy or use a weed wacker as it will aerosolize the poisonous oils.
Rubbing weeds on the skin can help.
False. Usually, prescription cortisone preparations are required to decrease the itching.
One way to protect against poison ivy is by keeping yourself covered outdoors.
True. However, urushiol can stick to your clothes, which your hands can touch, and then spread the oil to uncovered parts of your body. For uncovered areas, barrier creams are sometimes helpful. Learn to recognize poison ivy so you can avoid contact with it.



Poison Oak

Poison Sumac (wet marshy ares)
"OUCH! What Bit Me?"
Sometimes it’s easy to tell what bit you: maybe you reach down to swat at the bug and catch a glimpse of it. Sometimes though, it’s harder to tell. You might not notice the bite as it’s happening. Instead you don’t even realize you’ve been bitten until the spot starts to itch.
Although most bug bites and stings are harmless, some can be dangerous. This is especially true if you are allergic to the bug’s venom, or if the bug is carrying a disease. Most bug bites and stings can be safely treated at home with topical medication. However, sometimes a bug bite or sting could turn into something serious – particularly if you have been bitten or stung by many insects at the same time.
In the United States, it’s common to experience a bite or sting from the following types of bugs:
When weather permits, wear long sleeves and pants. They can add an extra layer of protection between you and your exposed skin. Light-colored clothing makes ticks easier to spot. Do a quick clothing and body check for ticks once you get inside.
Remember, insect repellants are your friend. The best ones contain DEET, like DEEP Woods OFF or ones that contain picaridin. Be sure to use any insect repellants according to the directions on the label.
For insect bites and stings that itch, you can put an ice pack on the spot and/or use an over-the-counter itch cream; for example, hydrocortisone. You may choose to instead take an oral antihistamine. Ice packs can also reduce swelling.
It’s important to pay attention to your symptoms. If you feel tired all the time, you have a headache, fever or body aches, or you develop a rash after a bug bite, see a board-certified dermatologist immediately.
Go to the emergency room immediately if you experience any of the following symptoms after a bug bite or sting:
You're more likely to get Lyme disease if you live or spend time in grassy and heavily wooded areas where ticks carrying Lyme disease thrive. It's important to take common-sense precautions in tick-infested areas.
Where you live or vacation can affect your chances of getting Lyme disease. So can your profession and the outdoor activities you enjoy. The most common risk factors for Lyme disease include:


A small, red bump, similar to the bump of a mosquito bite, often appears at the site of a tick bite or tick removal and resolves over a few days. This normal occurrence doesn't indicate Lyme disease.
However, these signs and symptoms can occur within a month after you've been infected:

If untreated, new signs and symptoms of Lyme infection might appear in the following weeks to months. These include:
Several weeks after infection, some people develop:
If you've been bitten by a tick and have symptoms, only a minority of tick bites lead to Lyme disease. The longer the tick remains attached to your skin, the greater your risk of getting the disease. Lyme infection is unlikely if the tick is attached for less than 36 to 48 hours.
If you think you've been bitten and have signs and symptoms of Lyme disease — particularly if you live in an area where Lyme disease is common — contact your doctor. Treatment for Lyme disease is more effective if begun early.
Visit your doctor even if signs and symptoms disappear — the absence of symptoms doesn't mean the disease is gone. Untreated, Lyme disease can spread to other parts of your body for several months to years after infection, causing arthritis and nervous system problems. Ticks can also transmit other illnesses, such as babesiosis and Colorado tick fever.
The best way to prevent Lyme disease is to avoid areas where deer ticks live, especially wooded, bushy areas with long grass. You can decrease your risk of getting Lyme disease with some simple precautions:
You want to use a sunscreen that offers to help protect your skin from sunburn, early skin aging and skin cancer.
Dr. Robinson recommends the following tips:
Sunscreens need to be reapplied every two hours and immediately after swimming or exercising. No sunscreen can filter out 100% of the suns damaging UVB/UVA rays, however, using an SPF of 30 or higher can block out 97% of the sun's UVB rays.
Some sunscreen products are also available in combination with moisturizers. However, while these products are convenient, remember that sunscreen needs to be reapplied every two hours. Unfortunately, cosmetics/foundations with sunscreen, sit on top of the skin, and do not always allow the active ingredients in the sunscreen to deliver their full protection.
Sunscreen may also be sold in combination with an insect repellent. The AAD recommends purchasing and using these products separately. The reason for this is, when combined in a single product, the insect repellent can reduce the effectiveness of the sunscreen. It is recommended by the the CDC, that sunscreen should always be applied first followed by insect repellent.
However, keep in mind, sunscreen alone cannot fully protect you. In addition to wearing sunscreen, we recommend taking the following steps:
Seeking shade, wearing protective clothing — including a lightweight, tight-weave, long-sleeved shirt & pants, a wide-brimmed hat, and sunglasses with UVA & UVB protection — and using an adequate amount of sunscreen are all important behaviors to reduce your risk of skin cancer.
As the United States declares Monkeypox outbreak a public health emergency, NYC declares a local state of emergency due to the outbreak. The American Academy of Dermatology & The World Health Organization have put together a Task Force to address the growing outbreak of Monkeypox (orthopoxvirus) in the US. Monkeypox is a contagious disease caused by the Monkeypox virus. US Map and case count on the 2020 outbreak here ...
Anyone can get Monkeypox. It is primarily spread through close, physical contact between people. In the current outbreak, the Monkeypox virus is spreading mainly during oral, anal and vaginal sex and other intimate contact, such as rimming, hugging, kissing, biting, cuddling and massage.
Previous outbreak experience elsewhere suggests that the elderly, those with weakened immune systems, pregnant people, and children under 8 years of age may be at heightened risk for severe outcomes. Smallpox vaccine may help protect you against Monkeypox. Although, immunity may wain with age, it is estimated that the smallpox vaccine can be over 80% effective in preventing Monkeypox. Howevver, the vaccine for smallpox was discontinued in 1972 when it was eradicated in the United States. So therefore, anyone who is 49 years of age or younger most likely did not receive a smallpox vaccine.
The best way to protect yourself from Monkeypox is to avoid sex and other intimate contact with multiple or anonymous partners.
If you choose to have sex or other intimate contact, the following can help reduce your risk:
How to Protect Yourself and Others from Monkeypox (PDF)
Most cases are mild. Symptoms usually start within two weeks of exposure, but in some cases they may not appear for up to 21 days. If you have a new, unexplained skin rash or lesion(s)/bump(s) on your skin and you don’t know what caused it and think you may have Monkeypox, it is important to see your dermatologist quickly to prevent exposing more people. Eligible New Yorkers who may have been exposed to Monkeypox can now get vaccinated to stay safe and slow the spread.
Some symptoms include:
A person is contagious until all sores have healed and a new layer of skin has formed, which can take two to four weeks.
If you start experiencing symptoms, isolate at home immediately, ideally stay in a separate area away from other family members and pets and talk to your dermatologist.
The following may increase your risk for severe disease if you are infected: HIV; other conditions that weaken your immune system; and a history of atopic dermatitis or eczema. If you have one of these conditions, it is especially important to see a provider right away, if you have symptoms.
To protect others while you are sick:
Not every rash is Monkeypox. Dr. Robinson can make a diagnosis of Monkeypox by looking at the pattern on the skin and where the rash appears. Please let the office know ahead of your visit that you have a "new unexplained rash or lesions" and think you may have monkeypox. If Dr. Robinson suspects Monkeypox may be the cause of the rash, he will swab the rash and send it to a lab, where a polymerase chain reaction test will be performed.
There is treatment approved for Monkeypox. Most people get better on their own without treatment. However, antiviral medication(s) (TPOXX) may help. Your provider will help you find out if you are eligible for antiviral treatment. They may be able to prescribe medicine and provide information about symptom relief.
Vaccination after possible exposure ... Eligible New Yorkers who may have been recently exposed to Monkeypox can get the JYNNEOS TM vaccine. Vaccine is free and available regardless of immigration status. Information about eligibility for the vaccine and appointments can be found here.
Getting vaccinated after a recent exposure may reduce the chance of you getting Monkeypox and it can reduce the symptoms if you do get it.
People should get two doses, at least four weeks apart.
Information about eligibility for the vaccine clinic and appointments can be found here.
JYNNEOS Vaccine for Monkeypox: Frequently Asked Questions (PDF)
Additionally, here is a link to a letter published in the Journal of the American Academy of Dermatology (JAAD) that explains the symptoms and features of monkeypox. For more information about monkeypox, visit the AAD website.

Molluscum Contagiosum rarely causes pain and will eventually clear on its own if you have a healthy immune system. They may go away without a trace, but this takes time, during which they can spread. On average, the bumps clear in 6-18 months without treatment. Sometimes, this takes longer and they can re-occur.
Avoid spreading molluscum to other parts of your body by:
Until the molluscum bumps go away, take precautions to help prevent spreading the molluscum virus to others. Watch what the American Academy of Dermatology recommends here ... https://youtu.be/klkQ2YcJHaw
Dr. Robinson also recommends:
Dr. Robinson offers these tips and others every day to help his patients feel more comfortable in their own skin.

