

Everyone has moles, sometimes 40 or more. Most people think of a mole as a dark brown spot, but moles have a wide range of appearance. At one time, a mole in a certain spot on the cheek of a woman was considered fashionable. These were called "beauty marks." Some were even painted on. However, not all moles are beautiful. They can be raised from the skin and very noticeable, they may contain dark hairs, or they may be dangerous.
Moles can appear anywhere on the skin. They are usually brown in color but can be skin colored and various sizes and shapes. The brown color is caused by melanocytes, special cells that produce the pigment melanin. Moles probably are determined before a person is born. Most appear during the first 20 years of life, although some may not appear until later. Sun exposure increases the number of moles, and they may darken. During the teen years and pregnancy, moles also get darker and larger and new ones may appear. Each mole has its own growth pattern. The typical life cycle of the common mole takes about 50 years. At first, moles are flat and tan like a freckle, or they can be pink, brown or black in color, Over time, they usually enlarge and some develop hairs. As the years pass, moles can change slowly, becoming more raised and lighter in color. Some will not change at all. Some moles will slowly disappear, seeming to fade away. Others will become raised far from the skin. They may develop a small "stalk" and eventually fall off or are rubbed off.
Recent studies have shown that certain types of moles have a higher-than-average risk of becoming cancerous. They may develop into a form of skin cancer known as malignant melanoma. Sunburns may increase the risk of melanoma. People with many more moles than average (greater than 100) are also more at risk for melanoma.
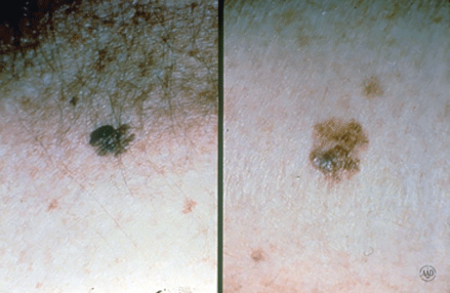
Moles are present at birth in about 1 in 100 people. They are called congenital nevi. These moles may be more likely to develop a melanoma than moles which appear after birth. Moles known as dysplastic nevi or atypical moles are larger than average (usually larger than a pencil eraser) and irregular in shape. They tend to have uneven color with dark brown centers and lighter, sometimes reddish, uneven border or black dots at edge. These moles often run in families. People with dysplastic nevi may have a greater chance of developing malignant melanoma and should be seen regularly by a dermatologist to check for any changes that might indicate skin cancer. Those susceptible should also learn to do regular self-examinations, looking for changes in the color, size or shape of their moles or the appearance of new moles. Sunscreen and protective clothing should be used to shield moles from sun exposure. Recognizing the early warning signs of malignant melanoma is important. Remember the ABCDs of melanoma when examining your moles: Read more here for Dr. Robinson in the News on Moles.
Melanoma is the most common type of cancer for young adults 25 to 29 years old, and the second most common type for adolescents and young adults 15-29 years old. Melanoma is a cancer of the pigment producing cells in the skin, known as melanocytes. Cancer is a condition in which one type of cell grows without limit in a disorganized fashion, disrupting and replacing normal tissues and their functions, much like weeds overgrowing a garden. Normal melanocytes reside in the outer layer of the skin and produce a brown pigment called melanin, which is responsible for skin color. Melanoma occurs when melanocytes become cancerous, and then grow and invade other tissues.
Melanoma begins on the surface of the skin where it is easy to see and treat. If given time to grow, melanoma can grow down into the skin, ultimately reaching the blood and lymphatic vessels, and spread around the body (metastasize), causing life-threatening illness. It is curable when detected early, but can be fatal if allowed to progress and spread. The goal is to detect melanoma early when it is still on the surface of the skin.
It is not certain how all cases of melanoma develop. Understanding what causes melanoma and whether you’re at high risk of developing the disease can help you prevent it or detect it early when it is easiest to treat and cure.
However, it is clear that excessive sun exposure, especially severe blistering sunburns early in life, can promote melanoma development. There is evidence that ultraviolet radiation used in indoor tanning equipment may cause melanoma. The risk for developing melanoma may also be inherited.
Anyone can get melanoma, but fair-skinned sun-sensitive people are at a higher risk. Since utraviolet radiation from the sun is a major culprit, people who tan poorly, or burn easily are at the greatest risk.
In addition to excessive sun exposure throughout life, people with many moles are at an increased risk to develop melanoma. The average person has around 30 moles, and most are without significance; however, people with more than 50 moles are at a greater risk. In addition to the number of moles, some people have moles that are unusual and irregular looking. These moles (nevi) are known as dysplastic or atypical moles. People with atypical moles are at increased risk of developing melanoma. Melanoma also runs in families. If a relative such as a parent, aunt or uncle had melanoma, other blood relatives are at an increased risk for melanoma.
The following factors help to identify those at risk for melanoma:
Anyone can develop melanoma, but people with one or more of the risk factors are more likely to do so. Annual skin examinations by a board-certified dermatologist can truly be life saving.
To help you find melanoma and other skin cancers early, dermatologists encourage everyone to learn the following:
The ABCDEs of melanoma
Learn to recognize a possible melanoma by learning these 5 warning signs.
How to perform a skin self-exam
Watch this short video to learn how to check your own skin for signs of melanoma and other skin cancers.





An estimated 2-3% of Americans suffer from excessive sweating of the underarms, or of the palms and soles of the feet. Sweating is embarrassing, it stains clothes, ruins romance and complicates business and social interactions. Severe cases can have serious practical consequences as well, making it hard for people who suffer from it to hold a pen, grip a car steering wheel or shake hands.
If left untreated these problems may continue throughout life. We can help!
Once other medical conditions have been ruled out, we offer a range of exciting treatment options – from prescription products to in-office treatments – to manage this condition. Dr. Robinson has many happy patients who were treated for Hyperhidrosis.
Although neurologic, endocrine, infectious, and other systemic diseases can sometimes cause hyperhidrosis, most cases occur in people who are otherwise healthy. Heat and emotions may trigger hyperhidrosis in some, but many who suffer from hyperhidrosis sweat nearly all their waking hours, regardless of their mood or the weather.
Through a systematic evaluation of causes and triggers of hyperhidrosis, followed by a judicious, stepwise approach to treatment, many people with this annoying disorder can sometimes achieve good results and improved quality of life.
The approach to treating excessive sweating generally proceeds as follows:
Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
The herpes simplex virus (HSV) causes blisters and sores often around the mouth, nose, genitals, and buttocks, but they can occur almost anywhere on the skin. HSV infections can be very annoying because they may reappear periodically. The sores may be painful and unsightly. For chronically ill people and newborn babies, the viral infection can be serious, but rarely fatal. There are two types of HSV - Type 1 and Type 2.
Often referred to as fever blisters or cold sores, infections are tiny, itchy, clear, fluid-filled blisters, often grouped together. They most often occur on the face.
Cold sores are caused by certain strains of the herpes simplex virus (HSV). HSV-1 usually causes cold sores. HSV-2 is usually responsible for genital herpes. But either type can spread to the face or genitals through close contact, such as kissing or oral sex. Shared eating utensils, razors and towels might also spread HSV-1.
Cold sores are contagious even if you don't see the sores. Cold sores spread from person to person by close contact, such as kissing.
There are two kinds of infections - primary and recurrent. Although most people get infected when exposed to the virus, only 10 percent will actually develop sores. The sores of a primary infection appear two to twenty days after contact with an infected person and can last from seven to ten days.
The number of blisters varies from a single to a group of blisters. Before the blisters appear, the skin may itch, sting, burn, or tingle. The blisters can break as a result of minor injury, allowing the fluid inside the blisters to ooze, crust & scab. Eventually, crusts fall off, leaving slightly red, healing skin.
The sores from the primary infection heal completely and rarely leave a scar. However, the virus that caused the infection remains in the body. It moves to nerve cells where it remains in a resting state.
People may then have a recurrence either in the same location as the first infection or in a nearby site. The infection may recur every few weeks or not at all.
Children under 5 years old may have cold sores inside their mouths and the lesions are commonly mistaken for canker sores. Canker sores involve only the mucous membrane and aren't caused by the herpes simplex virus.
Recurrent infections tend to be mild. They can be set off by a variety of factors including fever, sun exposure, a menstrual period, trauma (including surgery), or nothing at all.
Cold sores generally clear up without treatment. See your doctor if:
There's no cure for cold sores, but treatment can help manage outbreaks. Prescription antiviral pills or creams can help sores heal more quickly. And they may reduce the frequency, length and severity of future outbreaks.
Link to Domeboro instruction sheet
Hemangiomas/Angiomas are growths of blood vessels and other red spots which can be dilated blood vessels that take the form of a birthmark (Nevus Flameus).
Hemangiomas is a bright red birthmark that shows up at birth or in the first or second week of life. It looks like a rubbery bump and is made up of extra blood vessels in the skin. A hemangioma can occur anywhere on the body, but most commonly appears on the face, scalp, chest or back. It can grow out of proportion to the child for the first 8 months of life before the growth rate levels off. Therefore, it is important to evaluate these growths early especially if they are located around the eyes, mouth, genitals, scalp, neck or anus. Many hemangiomas disappear by age 5, and most are gone by age 10. The skin may be slightly discolored or raised after the hemangioma goes away.
Red bumps that we acquire with age or genetics are referred to as cherry angiomas. They often arise later in life and while not dangerous, can be considered unsightly. Their treatment can be simple and often requires no wound care enabling one to return to daily activities immediately.
A doctor can usually diagnose a hemangioma just by looking at it. Tests usually aren't needed.
A hemangioma is made up of extra blood vessels that group together into a dense clump. What causes the vessels to clump isn't known.
Hemangiomas occur more often in babies who are female, white and born prematurely.
Occasionally, a hemangioma can break down and develop a sore. This can lead to pain, bleeding, scarring or infection. Depending on where the hemangioma is situated, it may interfere with your child's vision, breathing, hearing or elimination, but this is rare.
Treating hemangiomas usually isn't necessary because they go away on their own with time. But if a hemangioma affects vision or causes other problems, treatments include medications or laser surgery:
If you're considering treatment for your child's hemangioma, weigh the pros and cons with your child's doctor. Consider that most infantile hemangiomas disappear on their own during childhood and that treatments have potential side effects.
Hand Eczema is dry skin of the hands. It is more common in the winter when the air holds less moisture and the cold wind increases water loss from the skin. It is worsened by frequent hand washing, using harsh soaps, not using moisturizer, and not using cotton-lined rubber gloves when doing work with detergents.
Genital warts affect the moist tissues of the genital area. They can look like small, flesh-colored and be flat or bumpy or have a cauliflower-like appearance. Some genital warts are so small they cannot be seen. They can cause pain, discomfort or itching. Genital warts, also known as venereal warts, or condylomata acuminata, are caused by the human papilloma virus (HPV). More than 100 types of HPV are known to exist. Low risk types (HPV 1, 2, and 3) cause warts on the hands, feet, and other parts of the body. The low risk strains - Types (6 and 11) can cause warts on the genitals or anus (genital warts), and other high risk strains - Types (HPV 16 and 18) can cause cancer of the cervix, external genitalia, vulva, and anus.
Genital warts are sexually transmitted disease (STD) and all partners should be checked thoroughly. They can also be seen in infants who have been delivered vaginally to mothers with HPV in their genital tracts; therefore, alternate methods of delivery should be considered.
Only a small percentage of people infected with HPV will develop genital warts. Many people are carriers of HPV who may never develop warts, but may still be able to pass HPV to their sexual partners. The incubation period from contracting HPV until the development of warts may be several months although some people may not develop warts for years after contact with HPV. People who have lower immunity due to cancer, AIDS, organ transplantation, immune suppressive medications, or certain other medications are more susceptible.
To diagnose this condition, your doctor will do the following:
Although HPV isn't curable in all cases, genital warts are treatable. You can also go extended periods of time without an outbreak, but it may not be possible to get rid of the warts forever. That's because genital warts are only a symptom of HPV, which may become a chronic, lifelong infection for some.
If you've developed genital warts, your doctor has a few options for treatment. The fastest way to remove them is through surgery or to freeze them off with liquid nitrogen. Some doctors might use an electric current or laser treatment to burn off the warts.
Genital warts can go away with treatment from your healthcare provider or with prescription medicine. If left untreated, genital warts may go away, stay the same, or grow in size or number. Cervical precancer treatment is available.
Your doctor may apply a mild acidic solution, called an acetowhite test, to your skin to help make genital warts more visible. It may cause a slight burning sensation.
If you have a vulva, your doctor may also need to perform a pelvic examination, because genital warts can occur deep inside your body.
While visible genital warts often go away with time, HPV itself can linger in your skin cells. This means you may have several outbreaks over the course of your life.
So managing symptoms is important because you want to avoid transmitting the virus to others. That said, genital warts can be passed on to others even when there are no visible warts or other symptoms.
You may wish to treat genital warts to relieve painful symptoms or to minimize their appearance. However, you can’t treat genital warts with over-the-counter (OTC) wart removers or treatments.
Your doctor may prescribe topical wart treatments that might include:
If visible warts don’t go away with time, you may need minor surgery to remove them. Your doctor can also remove warts through these procedures:
To help prevent genital warts, HPV vaccines, condoms, and other barrier methods are available:
If you think you have genital warts, talk with your doctor. They can determine if you have warts and what your best treatment options are.
In addition, it’s important to talk with your sexual partner. This may sound difficult, but being open about your condition can help you protect your partner from also getting an HPV infection and genital warts.
Genital warts are a complication of a low risk HPV infection that’s common and treatable. They can disappear over time, but treatment is essential in preventing their return and possible complications.
Laser treatment can be utilized for small facial areas or for the entire face. Recently, full face treatments have become increasingly popular. Many people suffer from larger broken capillaries on their nose and cheeks and will have medium and smaller vessels on other facial areas. A full-face treatment will improve the overall facial appearance by creating a more uniform skin color, and by smoothing the texture of the skin.
Light emitted from the handpiece safely passes through the outermost layers of skin in search of the targeted vascular or pigmented lesions. Without damaging the surrounding skin, the lasers intense light is absorbed by the targeted lesion. The light energy is then converted to heat and this initiates the process of eliminating the lesion. The treated lesion will gradually fade or diminish. In many cases, smaller vessels or pigmentation spots are eliminated in 2 to 4 treatments. Medium or larger vessels may take additional treatments.
The hand piece quickly advances across the skin delivering pulses to the treatment site. A full-face treatment typically lasts anywhere from 20 to 40 minutes. Smaller areas, such as the nose, can be treated in 15 minutes. In some cases a topical anesthetic cream is first applied to numb the treatment area. For a short period of time following treatment, a cold compress may be applied to soothe the possible appearance of slight swelling or redness of the skin. Treatments on the face, chest, neck, hands, legs, and abdomen are all done safely and quickly with laser technology.
During your consultation, your skin's condition will be evaluated and a customized treatment program will be suggested. In some cases only one or two treatments are required. However, in many cases three to five or more treatments will be required to achieve premium results. The number of treatment sessions will depend on the type of lesion to be treated, the location of the lesion on the body, and its size and color. In many cases, it is recommended that treatments applied to the face be repeated at 3 to 4 week intervals. The time intervals of your treatments will be determined during the consultation, where many of these issues and concerns may be addressed.
Eczema is a a type of dermatitis. The terms "eczema" and "dermatitis" are a group of skin conditions that cause skin inflammation and dry, itchy patches of skin. It’s a common condition that isn’t contagious. Symptoms of eczema can flare up if you contact an irritant or an allergen. There are treatments available to help you manage symptoms, but there isn’t a cure.
It’s possible to have more than one type of eczema at the same time.
Eczema can affect anyone at any age. Symptoms usually appear during childhood and last into adulthood. You might be more at risk of having eczema if you have a family history or a diagnosis of:
Eczema is common and affects more than 31 million Americans. Infants are prone to eczema, and 10% to 20% will have it. However, nearly half of all infants diagnosed with eczema outgrow the condition or have significant improvement as they get older.
Eczema doesn’t usually cause pain. If you scratch your skin, you could break the surface of your skin and create a sore, which could be painful. Some types of eczema, like contact dermatitis, cause a burning sensation and discomfort.
Eczema can look different on each person diagnosed with the condition. If you have a dark skin tone, an eczema rash can be purple, brown or gray. If you have a light skin tone, an eczema rash can look pink, red or purple.
While eczema can cause your immune system to overreact, it isn’t classified as an autoimmune condition. Research is ongoing to learn more about how eczema interacts with your immune system.
Q. Since this condition is associated with allergies, can certain foods be the cause?
A. Rarely (perhaps 10%). Although some foods may provoke atopic dermatitis, especially in infants and young children with asthma, eliminating those foods is rarely a cure. You should eliminate any foods that cause immediate severe reactions or welts.
Q. Are environmental causes important and should they be eliminated?
A. Rarely. The elimination of contact or airborne substances does not bring lasting relief. Occasionally, dust and dust-catching objects like feather pillows, down comforters, kapok pillows and mattresses, cat and dog dander, carpeting, drapes, some toys, wool, and other rough fabrics, can worsen atopic dermatitis.
Q. Are skin tests, like those given for hay fever or asthma, of any value in finding the causes?
A. Sometimes, but not as a rule. A positive test means allergy only about 20% of the time. If negative, the test is good evidence against allergy.
Q. Are shots (immunotherapy injections) such as those given for hay fever and other allergies useful?
A. Not usually. They may even make the skin condition worse in some patients.
Q. What should be done to treat this condition?
A. We will provide advice on avoiding irritating factors in creams and lotions; rough, scratchy, or tight clothing; and woolens. Rapid changes of temperature and any activity that causes sweating can aggravate atopic dermatitis. Proper bathing, moisturizing, and dealing with emotional upsets which may make the condition worse should be discussed.












Does your torn or expanding earring hole(s) cause you to worry about loosing an earring? If you are feeling limited because the hole is too big to accommodate some of your favorite earrings then Earlobe repair may be a solution for you. It is an easy in office procedure that restores your earlobe in about 30 minutes.
The dermatology practice of Bruce Robinson, M.D., offers advanced procedures including earlobe repair to not only improve your profile but restore self-confidence. If you would like to learn more about this exciting procedure or any of our other services, contact us today to schedule your initial consultation!
All patients have very distinctive reasons for considering earlobe repair. Accidents can occur at any given time in one’s life that may result in traumatized tissue. An earring could get caught up in a piece of clothing and cause a tear. Heavy or large jewelry can lead to stretched or enlarged earlobes with consistant wear. Whatever your reason may be, earlobe repair surgery can be performed to either remedy the earlobes natural appearance or to correct a tear, stretch, scar, or damage from a previous piercing or accident.
Usually 6 - 8 weeks you can re-pierce your ear(s). We offer ear piercing in our office.
We use the Coren PS ear piercer which painlessly pierces your earlobes and inserts a sterile, hypoallergenic, 24k gold ear stud.
Link to ear piercing instruction sheet

