

Just like a precious piece of jewlery or a beautiful piece of furniture, the skin can become dull, weathered and aged. With the modern age of dermatology one can restore the brightness, alleviate lines, get rid of dark marks, erase broken capillaries and scars with no social downtime and superior cosmetic results.
Cosmetic Consultation Reimbursement policy offered to all patients. Schedule an office visit to discuss your concerns and skincare goals with Dr. Robinson and the office visit cost will be applied to the future cost for the "consulted procedure". The "consulted procedure" must be completed within 30 days of your consult visit.
Skin Cancer is the cancer you can see! Yet skin cancer often goes undetected. With over 5 million cases of skin cancer diagnosed in the U.S. each year, skin cancer is America's most common cancer. More people are diagnosed with skin cancer each year in the U.S. than all other cancers combined.
Types of skin cancers include: Basal Cell Carcinoma, Squamous Cell Carcinoma, Melanoma and Merkel Cell Carcinoma, they are mainly caused by UV exposure to ultraviolet (UV) radiation from the sun. However, skin cancer can form anywhere on the body even if it is not exposed to the sun. All ethnicities and skin tones are at risk.
Dr. Bruce P. Robinson has pioneered a transformative new treatment option for the most common forms of skin cancer: Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC). His new and significant research in the treatment of Basal & Squamous cell carcinoma’s can be seen in the Archives of Dermatological Research, Utilizing fractional lasers and tirbanibulin ointment to treat squamous and basal cell carcinomas with a 99% cure rate to date and no recurrence
Basal Cell Carcinoma is the most common skin cancer and the number of reported cases in the U.S. is steadily increasing. It is also one of the easiest to spot and treat. Squamous Cell Carcinoma is the second most common skin cancer and Melanoma the third. Despite Melanoma being the third most common form of skin cancer, it accounts for 75% of all skin cancer deaths.
Squamous Cell Carcinoma is the second most common. An estimated 1.8 million cases are diagnosed each year in the U.S. which translates to about 205 cases every hour. SCC incidence has increased up to 200% in the past three decades.
Melanoma is the third most common and deadly cancers. Early detection is critical! In the past decade (2012-2022) the number of new invasive melanoma cases diagnosed annually increased by 31%. An estimated 197,700 cases of melanoma will be diagnosed in the U.S. in 2022 and 7,650 people will die of melanoma in 2022. (5,080 men & 2,570 women).
Merkel Cell Carcinoma is about three - five times more likely to be deadly than melanoma. Approximately 3,000 new cases of Merkel Cell Carcinoma are diagnosed annually in the U.S.
The good news is that skin cancer can be prevented, and it can almost always be cured when it’s found and treated early.
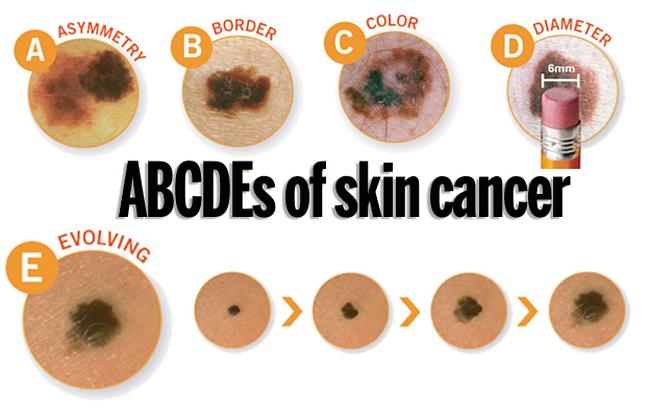
A change in your skin is the most common sign of skin cancer. This could be a new growth, a spot that doesn’t look like others on your body, a sore that doesn’t heal, or a change in a mole. The “ABCDE rule” can be used as a guide. The “ABCDE rule” can be used as a guide (see below).
Skin cancer isn't going to check itself out. Therefore, an annual skin check by a board-certified dermatologist and a monthly skin check by you is vital to good skin care. See something NEW, keep an eye out for any New moles or blemishes that have popped up, CHANGING, a leopard's spots don't change and neither should yours, always check if your spots are Changing in color, size, shape, or texture, or UNUSUAL, one of these things is not like the others ... look for spots that are unusual in outline or continuously itch, hurt, crust or bleed for more than 3 weeks. It could be skin cancer.
When these skin cancers are detected early, treatment often results in a cure. Be sure to schedule an yearly skin exam with your dermatologist and more often if you have a family history of skin cancer.
Take these simple steps today to protect your skin:
Dr. Bruce Robinson is advancing skin cancer treatment with innovative non-invasive techniques that provide superior outcomes compared to traditional methods like surgical excision and Mohs surgery. His approach uses fractional laser technology, which eliminates the need for downtime, scarring, or bleeding, while offering functional and cosmetic results that are more favorable than conventional treatments. This method enhances both patient care and quality of life by reducing the invasiveness of treatment and improving recovery. See Publication Here ...
Skin cancer is the most prevalent cancer in the United States. More than 3 million Americans are diagnosed with non-melanoma skin cancer(s), such as basal cell & squamous cell carcinoma each year. These two types of cancers are collectively known as keratinocyte carcinoma or (KC).
In individuals with a history of a prior KC, the risk of developing subsequent KC remains a significant concern.
Non-ablative fractional laser therapy has already demonstrated remarkable success with minimal downtime & discomfort as a gentle yet effective treatment of actinic keratosis (AK), the most common type of pre-cancerous skin conditions. Other benefits to using non-ablative fractional laser therapy is it's ability @ ameliorating photo damage, utilizing precise photothermolysis to stimulate collagen and elastin production, promote dermal wound healing & decreasing and improving hyperpigmentation, telangiectasias, skin tone, skin laxity, and tactile roughness. Now we can add treatment of certain skin cancers to the list.
Seborrheic Keratoses are often confused with warts or moles, but they are quite different. Seborrheic Keratoses are non-cancerous growths of the outer layer of skin. There may be just one growth or many which occur in clusters. They are usually brown, but can vary in color from light tan to black and range in size from a fraction of an inch in diameter to larger than a half-dollar. A main feature of Seborrheic Keratoses is their "waxy, pasted-on" appearance. They sometimes look like a dab of warm brown candle wax that has dropped onto the skin or like barnacles attached to the skin.
The exact cause of seborrheic keratoses is unknown; however, they seem to run in families. They are not caused by sunlight and can be found on both sun-exposed and non sun-exposed areas. Seborrheic Keratoses are more common and numerous with advancing age. Although Seborrheic Keratoses may first appear in one spot and seem to spread to another, they are not contagious.
Anyone may develop Seborrheic Keratoses. Some people develop many over time, while others develop only a few. As people age, they may simply develop more. Children rarely develop Seborrheic Keratoses. Seborrheic Keratoses may erupt during pregnancy, following estrogen therapy, or in association with other medical problems.
Seborrheic Keratoses are most often located on the chest or back, although they also can be found on the scalp, face, neck, or almost anywhere on the body. The growths usually begin one at a time as small, rough, itchy bumps which eventually thicken and develop a warty surface.
Seborrheic Keratoses are benign (non-cancerous) and are not serious. Unless they develop suddenly, they do not indicate a serious health problem. They may be unsightly, especially if they appear on the face. Removal may be recommended if they become large, irritated, itch, or bleed easily. A Seborrheic Keratosis may turn black and may be difficult to distinguish from skin cancer. Such a growth must be removed and biopsied (studied under a microscope) to determine if it is cancerous or not.
Creams, ointments, or other medication can neither cure nor prevent Seborrheic Keratoses. Most often Seborrheic Keratoses are removed by cryosurgery, curettage, or electrosurgery. Cryosurgery, liquid nitrogen, a very cold liquid gas, is applied to the growth with a cotton swab or spray gun to "freeze" it. A blister may form under the growth which dries into a scab-like crust. The Keratosis usually falls off within a few weeks. Occasionally, there will be a small dark or light spot that usually fades over time.
Curettage: The keratosis is scraped from the skin. An injection or spray is first used to anesthetize (numb) the area before the growth is removed (curetted). No stitches are necessary, and the minimal bleeding can be controlled by applying pressure or the application of a blood-clotting chemical.
Electrosurgery: The growth is anesthetized (numbed) and an electric current is used to burn the growth which is then scraped off.
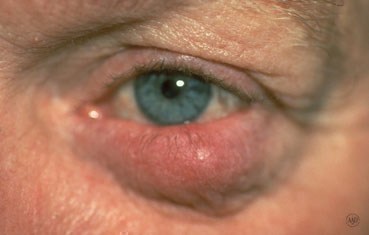
Seborrheic dermatitis is a common skin disorder that can be easily treated. This condition is a red, scaly, itchy rash most commonly seen on the scalp, sides of the nose, eyebrows, eyelids, skin behind the ears, and middle of the chest. Other areas, such as the navel (belly button), buttocks, skin folds under the arms, auxillary regions, breasts, and groin, may also be involved.
Your doctor will likely be able to determine whether you have seborrheic dermatitis by examining your skin. He or she may scrape off skin cells for examination (biopsy) to rule out conditions with symptoms similar to seborrheic dermatitis, including:
Dandruff appears as scaling on the scalp without redness. Seborrhea is excessive oiliness of the skin, especially of the scalp and face, without redness or scaling. Patients with Seborrhea may later develop Seborrheic Dermatitis. Seborrheic Dermatitis has both redness and scaling.
This condition is most common in three age groups - infancy, when it's called cradle cap, middle age, and the elderly. Cradle cap usually clears without treatment by age 8 to 12 months. In some infants, Seborrheic Dermatitis may develop only in the diaper area where it could be confused with other forms of diaper rash. When Seborrheic Dermatitis develops at other ages it can come and go. Seborrheic Dermatitis may be seasonally aggravated particularly in northern climates; it is common in people with oily skin or hair, and may be seen with acne or psoriasis. A yeast-like organism may be involved in causing Seborrheic Dermatitis.
Seborrheic Dermatitis may get better on its own, but with regular treatments, the condition improves quickly.
There is no way to prevent or cure Seborrheic Dermatitis. However, it can be controlled with treatment.
Medicated shampoos, creams and lotions are the main treatments for seborrheic dermatitis. Your doctor will likely recommend you try home remedies, such as over-the-counter dandruff shampoos, before considering prescription remedies. If home remedies don't help, talk with your doctor about trying these treatments.
Today, there are many treatment options which, when properly chosen for the specific type of scar and/or skin type, can greatly improve and repair your skin to its natural and more healthy state. These treatment options include surgical excision, laser skin resurfacing, laser skin rejuvenation, intense pulsed light skin rejuvenation, microdermabrasion, chemical peels, dermabrasion, cortisone injections, and bleaching or age defying softening topicals.
During your consultation, your skin type and scar will be evaluated and a customized treatment program will be developed. This may include a combination of treatments to optimize your results. In some cases, certain types of scars can only be improved and not completely eliminated. Your treatment expectations and results will be thoroughly discussed during your consultation.
This option is typically for scars that are deeply pitted, raised, or for older surgical scars that did not heal properly. The scar tissue is removed, followed by careful stitching of the skin to leave a much smaller or thinner scar line.
This treatment is excellent for acne scarring as well as sun damaged or aged skin. The laser vaporizes the damaged skin and commences the regeneration of fresh skin during the following weeks. The thermal damage to the deep tissue stimulates new skin growth, promoting a healthy new collagen layer as well.
Microdermabrasion is a non-surgical exfoliating treatment helpful for those unhappy with scars, acne scars, sun-damaged skin, pigmentation spots, stretch marks, fine lines, and rough skin. Treatment can be performed anywhere on the body. This treatment works for scarring especially when used in conjunction with other modalities.
This is a non-invasive approach in which the laser energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars.
Depending on the skin type and scar to be treated, a superficial, medium, or deep chemical peel may be recommended. In addition to removing the top layers of the epidermis, chemical peels are noted for their ability to stimulate collagen synthesis and aid in the production of new skin cells. Depending on the type of peel, multiple treatments may be required.
This is a non-invasive approach in which intense pulsed light energy penetrates the skin, damaging the deepest tissue layers. The damage causes the skin to repair itself and stimulates the production of collagen. As the underlying skin thickens, the top layers of the skin begin to contour more smoothly. Multiple treatments may be recommended. This treatment option works well in conjunction with microdermabrasion for certain scars and coarse, uneven skin texture.
By the time we reach our adult years, our skin has been exposed to rough childhood environmental damage, acne, chicken pox, scrapes, burns and numerous other phenomena. As part of the skin's natural healing process, a scar is formed when several layers of the skin have been damaged. Presently there are diverse treatment modalities available to address various forms of skin scarring. These treatments can dramatically reverse, improve, and renew your skin to it's natural, healthier state. Many patients seek solutions not only to achieve healthy-looking skin, but also to improve their image and self esteem.
Scabies is an infestation of the skin by the human itch mite. The tiny mites burrow into the upper layer of the skin where it lives and lays its eggs. It has infested humans for at least 2,500 years. It is often hard to detect, and causes a fiercely itchy skin condition. Dermatologists estimate that more than 300 million cases of scabies occur worldwide every year. The condition can strike anyone of any race or age, regardless of personal hygiene. The good news is that with better detection methods and treatments, scabies does not need to cause more than temporary distress.
The microscopic mite that causes scabies can barely be seen by the human eye. Being a tiny, eight-legged creature with a round body, the mite burrows in the skin. Within several weeks, the patient develops an allergic reaction causing severe itching; often intense enough to keep sufferers awake all night.
Human scabies is almost always caught from another person by close contact. It could be a child, a friend, or another family member. Everyone is susceptible. Scabies is not a condition only of low-income families and neglected children, although, it is more often seen in crowded living conditions with poor hygiene.
Attracted to warmth and odor, the female mite burrows into the skin, lays eggs, and produces toxins that cause allergic reactions. Larvae, or newly hatched mites, travel to the skin surface, lying in shallow pockets where they will develop into adult mites. If the mite is scratched off the skin, it can live in bedding for up to 24 hours or more. It may take up to a month before a person will notice the itching, especially in people with good hygiene and who bathe regularly.
The earliest and most common symptom of scabies is intense itching, especially at night. Little red bumps like hives, tiny bites, or pimples appear. In more advanced cases, a rash can spread slowly over a period of weeks or months and the skin may be crusty or scaly.
Scabies skin mite is about 0.4mm, just visible to the human eye
The scabies mite is very small, about the size of the tip of a needle and very difficult to see. It’s white to creamy-white in color. It has eight legs and a round body, which you can see if the mite is magnified. Scabies prefers warmer sites on the skin such as skin folds, where clothing is tight, between the fingers or under the nails, on the elbows or wrists, the buttocks or belt line, around the nipples, and on the penis. Mites also tend to hide in, or on, bracelets and watchbands, or the skin under rings. In children, the infestation may involve the entire body including the palms, soles, and scalp. The child may be tired and irritable because of loss of sleep from itching or scratching all night.
Bacterial infection may occur due to scratching. In many cases, children are treated because of infected skin lesions rather than for the scabies itself. Although treatment of bacterial infections may provide relief, recurrence is almost certain if the scabies infection itself is not treated.
Your healthcare provider must order a cream that contains a medicine called permethrin to treat scabies. The cream is applied to your whole body below your head, including the hands, palms, and soles of the feet.
In children with scabies, the cream may need to be applied to the scalp. Be sure that skin is clean, cool and dry before applying the cream.
Permethrin cream is left on the skin for eight to 14 hours and then washed off. (The cream is most often applied at night and washed off in the morning.)
Ivermectin is another option for treating scabies. This is an antiparasitic pill given in a single dose, followed by a second dose one to two weeks later.
If you’re pregnant or lactating, you shouldn’t use ivermectin. If your child weighs less than 35 pounds (15 kilograms), they shouldn’t use ivermectin.
Your provider might also suggest antihistamines, which can be taken by mouth and as a cream, to relieve itching. Your provider will also treat any type of infection that may be present.
The mites that cause scabies are killed after one treatment. The treatment doesn’t need to be repeated unless the infection doesn’t go away or comes back.
The itching may take two to four weeks to go away, even though the mites have been killed.
Red bumps on the skin should go away within four weeks after treatment.
You can prevent spreading scabies by:
Yes. You can get scabies any time that you come into close contact with an infected person.
No, scabies won’t go away on its own. If you don’t treat it, you’ll probably continue to spread the disease to other people. In addition, the constant itching will probably lead to constant scratching and will cause some type of bacterial infection of the skin.
Scabies is treatable, but they can be hard to get rid of completely. Certain forms of scabies are harder to treat, such as the crusted form. In addition, you might need more than one round of treatment to make sure all of the mites are gone.
If you have a rash and it’s so itchy that you can’t sleep, make sure you contact your healthcare provider. You may have scabies, which is an infectious disease. You and other people close to you should be tested and treated. You’ll want to schedule an appointment with Dr. Robinson if you have any kind of skin rash that doesn’t go away and that causes problems for you. Scabies, like many other types of red itchy rashes, can be treated successfully.
Rosacea is a common skin disease that causes redness, papules, and swelling on the face. Often referred to as adult acne, rosacea frequently begins as a tendency to flush or blush easily. It may progress to persistent redness in the center of the face that may gradually involve the cheeks, forehead, chin, and nose. The eyes, ears, chest, and back may also be involved. With time, small blood vessels and tiny pimples begin to appear on and around the reddened area; however, unlike acne, there are no blackheads.
When rosacea first develops, the redness may come and go. Some people may flush or blush and never form pustules or papules. Small dilated vessels may also be present. However, when the skin doesn't return to its normal color, and when other symptoms such as pimples and enlarged blood vessels become visible, it's best to seek advice from a board-certified dermatologist. The condition may last for years, rarely reverse itself, and can become worse without treatment.
Small red bumps, some of which may contain pus, appear on the face. These may be accompanied by persistent redness and the development of many tiny blood vessels on the surface of the skin.
In more advanced cases, a condition called rhinophyma may develop. The oil glands enlarge causing a bulbous, red nose, and puffy cheeks. Thick bumps may develop on the lower half of the nose and nearby cheeks. Rhinophyma occurs more commonly in men.
Anyone can get Rosacea. It is more common in fair skinned adults between the ages of 30 and 50. Since it may be associated with menopause, women are affected more often than men and may likely have an extreme sensitivity to cosmetics. In people of color, studies show that early symptoms can often be missed and may be under diagnosed because dark skin can mask facial redness. Few children get rosacea, but it is worth considering if the signs and symptoms are there.
Tips for Rosacea Patients
Many people with Rosacea are unfamiliar with it and do not recognize it in its early stages. Identifying the disease is the first step to controlling it. Self-diagnosis and treatment are not recommended since some over-the-counter skin products may make the problem worse.
Dermatologists often recommend a combination of treatments tailored to the individual patient. These treatments can stop the progress of rosacea and sometimes reverse it.
The key to successful management of Rosacea is early diagnosis and treatment. Rosacea can be treated and controlled if medical advice is sought in the early stages. When left untreated, Rosacea will get worse and may be more difficult to treat.





Pruritus is an itch or a sensation that makes a person want to scratch. Pruritus can cause discomfort and be frustrating. If it is severe, it can lead to sleeplessness, anxiety, and depression. The exact cause of an itch is unknown. It is a complex process involving nerves that respond to certain chemicals like histamine that are released in the skin, and the processing of nerve signals in the brain. Pruritus can be a part of skin diseases, internal disorders, or due to faulty processing of the itch sensation within the nervous system.
There are many skin diseases like urticaria (hives), varicella (chicken pox), and eczema which may have itching associated with a rash. Some skin conditions only have symptoms of pruritus without having an obvious rash. Dry skin can itch, especially in the winter, with no visual signs of a rash. Some parasitic infestations such as scabies and lice may be very itchy. Itchy, pigmented moles may be a sign of a malignant change.
Pruritus may be a manifestation of an internal condition. The most common example is kidney failure. Some types of liver disease like hepatitis, thyroid disease including both hyper (too much) and hypo (too little) thyroid hormone levels, some blood disorders such as lymphomas, iron deficiency anemia, polycythemia vera, multiple myeloma, and neurologic conditions such as pinched nerves and post herpetic neuralgia can cause itch. Infectious diseases like HIV can cause severe itching.
Varicella
Eczema
Scabies
Often the dermatologist will be able to diagnose these conditions with an examination; however, to determine a specific cause of the itch, a blood test, skin scraping, or biopsy may be needed to help make the diagnosis. If the itch is due to a skin disease such as hives or eczema, treatment of the skin disease, itself, with prescription topical medications and/or oral antihistamines generally relieves the itch. If the itch is secondary to an internal disease, patients may require treatment of the disease, oral medication, or occasionally ultraviolet light therapy to relieve the itch.
Sometimes, the dermatologist will prescribe a cooling topical lotion or cream and/or an oral medication to relieve the itch. Pruritus is often disrupting and difficult to control but usually responds well to treatment. While a specific identifying cause for the itch may not be found, an appropriate work-up to exclude internal disease should be completed.
Although there are many causes for pruritus, some basics apply to most treatments:
Poison ivy, poison oak, and poison sumac are the most common cause of allergic reactions in the United States. Each year 10 to 50 million Americans develop an allergic rash after contact with these poison plants.
Poison ivy, poison oak, and poison sumac grow almost everywhere in the United States, except Hawaii, Alaska, and some desert areas in the Western U.S. poison ivy usually grows east of the Rocky Mountains and in Canada. Poison oak grows in the Western United States, Canada, Mexico (western poison oak), and in the Southeastern states (eastern poison oak). poison sumac grows in the Eastern states and southern Canada.
In the West, this plant may grow as a vine but usually is a shrub. In the East, it grows as a shrub. It has three leaflets to form its leaves in the shape of an oak tree leaf.
Grows as a vine in the East, Midwest and South. In the far Northern and Western United States, Canada and around the Great Lakes, it grows as a shrub. Each leaf has three leaflets.
Grows in standing water in peat bogs in the Northeast and Midwest and in swampy areas in parts of the Southeast. Each leaf has seven to 13 leaflets.
Poison Plant rash is an allergic contact dermatitis caused by contact with oil called urushiol. Urushiol is found in the sap of poison plants like Poison Ivy, Poison Oak, and Poison Sumac. It is colorless or pale yellow oil that oozes from any cut or crushed part of the plant, including the roots, stems, and leaves. After exposure to air, urushiol turns brownish-black. Damaged leaves look like they have spots of black enamel paint making it easier to recognize and identify the plant. Contact with urushiol can occur in three ways:
When urushiol gets on the skin, it begins to penetrate in minutes. A reaction appears usually within 12 to 48 hours. There is severe itching, redness, and swelling, followed by blisters. The rash is often arranged in streaks or lines where the person brushed against the plant. In a few days, the blisters become crusted and take 10 days or longer to heal.
Poison plant dermatitis can affect almost any part of the body. The rash does not spread by touching it, although it may seem to when it breaks out in new areas. This may happen because urushiol absorbs more slowly into skin that is thicker such as on the forearms, legs, and trunk.
Sensitivity develops after the first direct skin contact with urushiol oil. An allergic reaction seldom occurs on the first exposure. A second encounter can produce a reaction which may be severe. About 85 percent of all people will develop an allergic reaction when adequately exposed to poison ivy. This sensitivity varies from person to person. People who reach adulthood without becoming sensitive have only a 50 percent chance of developing an allergy to poison ivy. However, only about 15 percent of people seem to be resistant.
Identifying the poison ivy plant is the first step in avoiding the rash. The popular saying of leaves of three, let it be; is a good rule of thumb for Poison Ivy and Poison Oak, but is only partly correct. A more exact saying would be leaflets of three, beware of me; because each leaf has three leaflets. Poison sumac, however, has a row of paired leaves. The middle or end leaf is on a longer stalk than the other leaves. This differs from most other three-leaf look alikes.
Poison Ivy has different forms. It grows as vines or low shrubs. Poison Oak, with its oak-like leaves, is a low shrub in the East and can be a low or high shrub in the West. Poison sumac is a tall shrub or small tree. The plants also differ in where they grow. Poison Ivy grows in fertile, well-drained soil. Western Poison Oak needs a great deal of water, and Eastern Poison Oak prefers sandy soil but sometimes grows near lakes. Poison Sumac tends to grow in standing water, such as peat bogs.
These plants are common in the spring and summer. When they grow, there is plenty of sap and the plants bruise easily. The leaves may have black marks where they have been injured. Although Poison Ivy rash is usually a summer complaint, cases may occur in winter when people are cleaning their yards and burning wood with urushiol on it, or when cutting Poison Ivy vines to make wreaths.
It is important to recognize these toxic plants in all seasons. In the early fall, the leaves can turn colors such as yellow or red when other plants are still green. The berry-like fruit on the mature female plants also changes color in fall, from green to off-white. In the winter, the plants lose their leaves. In the spring, Poison Ivy has yellow-green flowers.
Prevent the misery of Poison Ivy by looking out for the plant and staying away from it. You can destroy these plants with herbicides in your own backyard, but this is not practical elsewhere. If you are going to be where you know poison ivy likely grows, wear long pants, long sleeves, boots, and gloves. Remember that the plant's nearly invisible oil, urushiol, sticks to almost all surfaces, and does not dry. Do not let pets run through wooded areas since they may carry home urushiol on their fur. Because urushiol can travel in the wind if it burns in a fire, do not burn plants that look like Poison Ivy.
Barrier skin creams such as a lotion containing bentoquatum offer some protection before contact with Poison Ivy, Poison Oak, or Poison Sumac. Over-the-counter products prevent urushiol from penetrating the skin. Ask your dermatologist for details.
If you think you've had a brush with Poison Ivy, Poison Oak, or Poison Sumac, follow these simple ste
Scratching Poison Ivy blisters will spread the rash.
False. The fluid in the blisters will not spread the rash. The rash is spread only by urushiol. For instance, if you have urushiol on your hands, scratching your nose or wiping your forehead will cause a rash in those areas even though leaves did not contact the face. Avoid excessive scratching of your blisters. Your fingernails may carry bacteria that could cause an infection.
Poison Ivy rash;
False. The rash is a reaction to urushiol. The rash cannot pass from person to person; only urushiol can be spread by contact.
Once allergic, always allergic to Poison Ivy.
False. A person's sensitivity changes over time, even from season to season. People who were sensitive to Poison Ivy as children may not be allergic as adults.
Dead Poison Ivy plants are no longer toxic.
False. Urushiol remains active for up to several years. Never handle dead plants that look like Poison Ivy or use a weed wacker as it will aerosolize the poisonous oils.
Rubbing weeds on the skin can help.
False. Usually, prescription cortisone preparations are required to decrease the itching.
One way to protect against poison ivy is by keeping yourself covered outdoors.
True. However, urushiol can stick to your clothes, which your hands can touch, and then spread the oil to uncovered parts of your body. For uncovered areas, barrier creams are sometimes helpful. Learn to recognize poison ivy so you can avoid contact with it.



Poison Oak

Poison Sumac (wet marshy ares)
Pityriasis Rosea is a rash that occurs most commonly in people between the ages of 10 and 35, but may occur at any age. The rash can last from several weeks to several months. Usually there are no permanent marks as a result of this condition, although some darker-skinned persons may develop long-lasting flat brown spots that eventually fade. It may occur at anytime of year, but Pityriasis Rosea is most common in the spring and fall.
Pityriasis rosea usually begins with a large, scaly, pink patch on the chest or back, which is called a herold or mother patch. It is frequently confused with ringworm, but antifungal creams do not help because it is not a fungus.
Within a week or two, more pink patches appear on the chest, back, arms, and legs. Patches may also occur on the neck, but rarely on the face. The patches are oval and may form a pattern over the back that resembles the outline of a Christmas tree. Sometimes the disease can produce a very severe and widespread skin eruption. About half the patients will have some itching, especially when they become warm. Physical activities like jogging and running, or bathing in hot water, may cause the rash to temporarily worsen or become more obvious. There may be other symptoms including fatigue and aching. The rash usually fades and disappears within six to eight weeks, but can sometimes last much longer.
The cause is unknown. Pityriasis Rosea is not a sign of any internal disease, nor is it caused by a fungus, a bacteria, or an allergy. There is recent evidence suggesting that it may be caused by a virus since the rash resembles certain viral illnesses, and occasionally a person feels slightly ill for a short while just before the rash appears. However, this has not been proven. Pityriasis rosea does not seem to spread from person to person and it usually occurs only once in a lifetime.
Pityriasis rosea affects the back, neck, chest, abdomen, upper arms, and legs, but the rash may differ from person to person making the diagnosis more difficult. The numbers and sizes of the spots can also vary, and occasionally the rash can be found in an unusual location such as the lower body, or on the face. This usually occurs in older individuals. Fungal infections, like ringworm, may resemble this rash. Reactions to certain medications, such as antibiotics, water pill, and heart medications can also look the same as Pityriasis Rosea.
The dermatologist may order blood tests, scrape the skin, or take a sample from one of the spots (skin biopsy), to examine under a microscope in order to make the diagnosis.
Pityriasis rosea often requires no treatment and it usually goes away by itself. However, treatment may include external or internal medications for itching and soothing medicated lotions and lubricants may be prescribed. Lukewarm rather than hot baths may be suggested. Ultraviolet light treatments given under the supervision of a dermatologist may be helpful.
Occasionally, anti-inflammatory medications such as corticosteroid may be necessary to stop itching or make the rash go away. Patients should be reassured that this disease is not a dangerous skin condition even if it occurs during pregnancy.
Remember that Pityriasis Rosea is a common skin disorder and is usually mild. Most cases usually do not need treatment and fortunately, even the most severe cases eventually go away.

